The student's skills necessary for the implementation of empirical CPD Justification of the relevance of the research Determination of the subject and object of empirical research (EI) Formulation of the goal and objectives of EI Planning of EI and forecasting the reliability of expected results Selection of methods and selection of methods for testing the hypothesis of empirical research Practical development of research methods Statistical processing of EI data Interpretation of the results obtained Formulation of conclusions and recommendations Correct design of the thesis
 Design of work Page format - A 4, font - 14, interstr. spacing - 1, 5. Alignment in width, left indent - 1, 5. Text should be placed on one side of a sheet of paper, observing the following margins: left - 30 mm, right - 15 mm, top - 20 mm, bottom - 20 mm ...
Design of work Page format - A 4, font - 14, interstr. spacing - 1, 5. Alignment in width, left indent - 1, 5. Text should be placed on one side of a sheet of paper, observing the following margins: left - 30 mm, right - 15 mm, top - 20 mm, bottom - 20 mm ...
 The title page is the first page of the WRC / KR and is drawn up in accordance with the established template. Not numbered
The title page is the first page of the WRC / KR and is drawn up in accordance with the established template. Not numbered

 Abstract The abstract is drawn up at the very last moment (after the completion of the work on the CD), however, the work follows the title page The abstract indicates: 1. The volume of pages The number of figures in the Diagrams of the Appendix Tables of the Sources 2. The list of keywords, which together give an idea of \u200b\u200bthis work 3 The object of research is determined The subject of research The purpose of the thesis 4. The methods of research activity used. The page is not numbered The tasks in the abstract are not formulated !!! For example: When developing and solving the set goal, methods were used - observation, comparison, analysis of theoretical and practical material.
Abstract The abstract is drawn up at the very last moment (after the completion of the work on the CD), however, the work follows the title page The abstract indicates: 1. The volume of pages The number of figures in the Diagrams of the Appendix Tables of the Sources 2. The list of keywords, which together give an idea of \u200b\u200bthis work 3 The object of research is determined The subject of research The purpose of the thesis 4. The methods of research activity used. The page is not numbered The tasks in the abstract are not formulated !!! For example: When developing and solving the set goal, methods were used - observation, comparison, analysis of theoretical and practical material.
 An example of an abstract of a thesis Abstract Thesis is written on 92 pages, the work contains 8 tables, 10 appendices, 5 diagrams, 8 figures. The list of key words that give an idea of \u200b\u200bthe content of this work: diseases leading to the threat of terminal conditions, the structure of the FAP, regulatory and legal acts regulating the activities of a paramedic in this pathology, morbidity, prevention. The object of research in the thesis is the tactics of a paramedic during cardiopulmonary resuscitation; The subject of the research is the identification of factors affecting the effectiveness of cardiopulmonary resuscitation; The main goal of the course work is to substantiate the list of necessary techniques and tools that increase the effectiveness of cardiopulmonary resuscitation at the prehospital stage; When developing and solving the set goal, methods were used - observation, comparison, analysis of theoretical and practical material.
An example of an abstract of a thesis Abstract Thesis is written on 92 pages, the work contains 8 tables, 10 appendices, 5 diagrams, 8 figures. The list of key words that give an idea of \u200b\u200bthe content of this work: diseases leading to the threat of terminal conditions, the structure of the FAP, regulatory and legal acts regulating the activities of a paramedic in this pathology, morbidity, prevention. The object of research in the thesis is the tactics of a paramedic during cardiopulmonary resuscitation; The subject of the research is the identification of factors affecting the effectiveness of cardiopulmonary resuscitation; The main goal of the course work is to substantiate the list of necessary techniques and tools that increase the effectiveness of cardiopulmonary resuscitation at the prehospital stage; When developing and solving the set goal, methods were used - observation, comparison, analysis of theoretical and practical material.
 Requirements for choosing a topic for a term paper / thesis Specificity of the topic The subject and object of research should be clear from the title of the work.The title of the work should correspond to the research hypothesis or the purpose of the research.In the case of long titles, they are best readable by the use of additional explanatory and clarifying comments after the colon. For example: "Teenage crisis among girls raised in single-parent families: individual characteristics"
Requirements for choosing a topic for a term paper / thesis Specificity of the topic The subject and object of research should be clear from the title of the work.The title of the work should correspond to the research hypothesis or the purpose of the research.In the case of long titles, they are best readable by the use of additional explanatory and clarifying comments after the colon. For example: "Teenage crisis among girls raised in single-parent families: individual characteristics"
 Object of research The object of research is a fragment of reality that is being studied or a field of activity. Object is a process or phenomenon that generates a problem situation, which the author has chosen for research. The object of the research answers the question: “What are we considering? »For example: R&D: Features of the professional activity of a nurse in bronchial asthma. Object of research: The activity of a nurse in therapeutic diseases in a hospital / and, or polyclinic
Object of research The object of research is a fragment of reality that is being studied or a field of activity. Object is a process or phenomenon that generates a problem situation, which the author has chosen for research. The object of the research answers the question: “What are we considering? »For example: R&D: Features of the professional activity of a nurse in bronchial asthma. Object of research: The activity of a nurse in therapeutic diseases in a hospital / and, or polyclinic
 Subject of research The subject of research is certain aspects or relationships of an object, processes, states or properties of phenomena or people, functions and characteristics of individual phenomena, connections and their influence on each other. It is on the subject of research that the author's main attention is directed, it is the subject that determines the topic of the work. For his research (subject), the goal and objectives are formulated. For example: R&D: Features of professional activity of a nurse in bronchial asthma. Subject of research: Features of the professional activity of a nurse with asthma in a hospital and, or polyclinic
Subject of research The subject of research is certain aspects or relationships of an object, processes, states or properties of phenomena or people, functions and characteristics of individual phenomena, connections and their influence on each other. It is on the subject of research that the author's main attention is directed, it is the subject that determines the topic of the work. For his research (subject), the goal and objectives are formulated. For example: R&D: Features of professional activity of a nurse in bronchial asthma. Subject of research: Features of the professional activity of a nurse with asthma in a hospital and, or polyclinic
 Purpose of research The purpose of the work characterizes its expected result. The goal directly depends on the topic. For example: R&D: Features of the professional activity of a nurse in bronchial asthma. Purpose of the work: To substantiate the list of necessary techniques and tools that optimize nursing activities in providing assistance to patients with asthma; to conduct approbation in the course of educational / industrial practice and formulate practical recommendations for improving SS in bronchial asthma
Purpose of research The purpose of the work characterizes its expected result. The goal directly depends on the topic. For example: R&D: Features of the professional activity of a nurse in bronchial asthma. Purpose of the work: To substantiate the list of necessary techniques and tools that optimize nursing activities in providing assistance to patients with asthma; to conduct approbation in the course of educational / industrial practice and formulate practical recommendations for improving SS in bronchial asthma
 Research objectives are the choice of ways and means to achieve the goal. Specify the goal. Theoretical problems are usually solved by analysis, synthesis, search for similar and different, abstraction and generalization, classification and systematization of theoretical and empirical data available in the literature. Empirical problems are solved by collecting and analyzing data obtained using empirical methods, such as observation, experiment, conversation, questioning, measurement, as well as methods of qualitative and quantitative processing of these data, such as typology, correlation, comparison, factorization. To achieve the goal in the course / thesis work, no more than 5 tasks are set
Research objectives are the choice of ways and means to achieve the goal. Specify the goal. Theoretical problems are usually solved by analysis, synthesis, search for similar and different, abstraction and generalization, classification and systematization of theoretical and empirical data available in the literature. Empirical problems are solved by collecting and analyzing data obtained using empirical methods, such as observation, experiment, conversation, questioning, measurement, as well as methods of qualitative and quantitative processing of these data, such as typology, correlation, comparison, factorization. To achieve the goal in the course / thesis work, no more than 5 tasks are set
 An example of the formulation of the goal and objectives of the thesis R&D: Features of the professional activity of a nurse in bronchial asthma. Purpose of the work: To substantiate the list of necessary techniques and tools that optimize nursing activity in providing care to patients with asthma Objectives: 1. To analyze the normative documentation governing the tactics of a nurse with asthma 2. To analyze the peculiarities of the work of a nurse with asthma in a therapeutic hospital of the GBUZ YAO Pereslavskaya CRH "3. To analyze the peculiarities of the work of a nurse with asthma in a polyclinic of GBUZ YaO" Pereslavskaya CRH "4. Give recommendations on how to optimize the activities of a nurse in managing patients with asthma
An example of the formulation of the goal and objectives of the thesis R&D: Features of the professional activity of a nurse in bronchial asthma. Purpose of the work: To substantiate the list of necessary techniques and tools that optimize nursing activity in providing care to patients with asthma Objectives: 1. To analyze the normative documentation governing the tactics of a nurse with asthma 2. To analyze the peculiarities of the work of a nurse with asthma in a therapeutic hospital of the GBUZ YAO Pereslavskaya CRH "3. To analyze the peculiarities of the work of a nurse with asthma in a polyclinic of GBUZ YaO" Pereslavskaya CRH "4. Give recommendations on how to optimize the activities of a nurse in managing patients with asthma
 The table of contents contains all the headings of the sections of the CD with the indication of the pages from which they begin. not numbered
The table of contents contains all the headings of the sections of the CD with the indication of the pages from which they begin. not numbered
 The introduction substantiates the relevance of the chosen topic, determines the goals and objectives of the research, the subject and object, research methods, indicates the basis of the work
The introduction substantiates the relevance of the chosen topic, determines the goals and objectives of the research, the subject and object, research methods, indicates the basis of the work
 INTRODUCTION Relevance of the topic Object of research Subject of research Purpose of the thesis Objectives of the thesis Base of work
INTRODUCTION Relevance of the topic Object of research Subject of research Purpose of the thesis Objectives of the thesis Base of work
 The relevance of the research topic is the degree of its importance at the moment and in this situation for solving these problems or tasks Relevance is revealed in the introduction Coverage of relevance should not be verbose Volume for the thesis - one page
The relevance of the research topic is the degree of its importance at the moment and in this situation for solving these problems or tasks Relevance is revealed in the introduction Coverage of relevance should not be verbose Volume for the thesis - one page
 Introduction (example) The number of people who die annually in Russia from sudden cardiac arrest (SCF) is comparable to the population of a large city and amounts to about 300,000 cases. According to official statistics, in Europe and America, in 1-5 cases for every thousand hospitalized patients, there is a need for cardiopulmonary resuscitation (CPR) measures. According to the statistics of the World Health Organization, 30 people suddenly die per one million population per week. In the United States, timely and proper CPR can save 100,000 to 200,000 lives annually. Sudden cardiac death accounts for 15-20% of all nonviolent deaths among residents of developed countries and can overtake even an absolutely healthy person without preliminary signs of cardiovascular disease, suddenly and without regard to age. An exhaustive answer to the question of the reasons for this phenomenon still does not exist. About 75% of cases of VOS occur at home, at work, in places of recreation, and only 25% of cases - in hospitals. Without first aid, about 91% of those affected by SCI die before being admitted to hospital. Thus, it is the paramedic of an ambulance or FAP who should provide assistance at the site of the development of clinical death in full. The pattern is obvious: the earlier assistance is started, the higher the likelihood of a person being saved, therefore, resuscitation measures at the scene of an accident should be the most effective and timely. Considering the above, a problem arises: the organization of the effective activity of a paramedic at the emergency room and FAP during cardiopulmonary resuscitation. The solution to this problem is one of the main ways to reduce mortality and significantly increase the effectiveness of medical care to the population. The purpose of the study is to substantiate the list of necessary techniques and tools used by a paramedic to increase the effectiveness of CPR. The object of the study is the tactics of a paramedic during CPR. The subject of the research is the identification of factors affecting the effectiveness of CPR. In accordance with the purpose, object and subject of the study, the following tasks are set: 1. Analyze the normative documentation governing the tactics of a paramedic during CPR. 2. Analyze the prevalence of diseases that can lead to the development of terminal conditions at FAP. 3. Analyze the statistics of the EMS on the conduct of resuscitation measures and their effectiveness. 4. Make suggestions on techniques and tools that increase the effectiveness of the paramedic CPR. Base of work: Medyaginsky feldsher-obstetric station, GUZ YaO SSMP.
Introduction (example) The number of people who die annually in Russia from sudden cardiac arrest (SCF) is comparable to the population of a large city and amounts to about 300,000 cases. According to official statistics, in Europe and America, in 1-5 cases for every thousand hospitalized patients, there is a need for cardiopulmonary resuscitation (CPR) measures. According to the statistics of the World Health Organization, 30 people suddenly die per one million population per week. In the United States, timely and proper CPR can save 100,000 to 200,000 lives annually. Sudden cardiac death accounts for 15-20% of all nonviolent deaths among residents of developed countries and can overtake even an absolutely healthy person without preliminary signs of cardiovascular disease, suddenly and without regard to age. An exhaustive answer to the question of the reasons for this phenomenon still does not exist. About 75% of cases of VOS occur at home, at work, in places of recreation, and only 25% of cases - in hospitals. Without first aid, about 91% of those affected by SCI die before being admitted to hospital. Thus, it is the paramedic of an ambulance or FAP who should provide assistance at the site of the development of clinical death in full. The pattern is obvious: the earlier assistance is started, the higher the likelihood of a person being saved, therefore, resuscitation measures at the scene of an accident should be the most effective and timely. Considering the above, a problem arises: the organization of the effective activity of a paramedic at the emergency room and FAP during cardiopulmonary resuscitation. The solution to this problem is one of the main ways to reduce mortality and significantly increase the effectiveness of medical care to the population. The purpose of the study is to substantiate the list of necessary techniques and tools used by a paramedic to increase the effectiveness of CPR. The object of the study is the tactics of a paramedic during CPR. The subject of the research is the identification of factors affecting the effectiveness of CPR. In accordance with the purpose, object and subject of the study, the following tasks are set: 1. Analyze the normative documentation governing the tactics of a paramedic during CPR. 2. Analyze the prevalence of diseases that can lead to the development of terminal conditions at FAP. 3. Analyze the statistics of the EMS on the conduct of resuscitation measures and their effectiveness. 4. Make suggestions on techniques and tools that increase the effectiveness of the paramedic CPR. Base of work: Medyaginsky feldsher-obstetric station, GUZ YaO SSMP.
 The main part is informative in nature, it solves the assigned tasks, describes the course and results of scientific and analytical work.
The main part is informative in nature, it solves the assigned tasks, describes the course and results of scientific and analytical work.

 The practical significance of the research lies in the possibility of using its results for solving practical problems. Here the student needs to show how the scientific results obtained by him can be useful for solving practical problems in a certain field of activity.The practical significance of the research should logically follow from the research itself
The practical significance of the research lies in the possibility of using its results for solving practical problems. Here the student needs to show how the scientific results obtained by him can be useful for solving practical problems in a certain field of activity.The practical significance of the research should logically follow from the research itself
 Practical part of the CD The number of paragraphs of the practical part most often corresponds to the number of tasks. A separate paragraph of the chapter is allocated for the solution of each practical problem. At the end of each paragraph, a conclusion is made Practical part of the course work: Drawing up a questionnaire to identify risk factors for a disease in a patient Drawing up a patient care plan Drawing up a plan for preparing a patient for SIA Drawing up reminders for a patient on therapeutic nutrition, physical activity, rules for taking prescribed drugs Drawing up recommendations for relatives on the organization of patient care at home
Practical part of the CD The number of paragraphs of the practical part most often corresponds to the number of tasks. A separate paragraph of the chapter is allocated for the solution of each practical problem. At the end of each paragraph, a conclusion is made Practical part of the course work: Drawing up a questionnaire to identify risk factors for a disease in a patient Drawing up a patient care plan Drawing up a plan for preparing a patient for SIA Drawing up reminders for a patient on therapeutic nutrition, physical activity, rules for taking prescribed drugs Drawing up recommendations for relatives on the organization of patient care at home
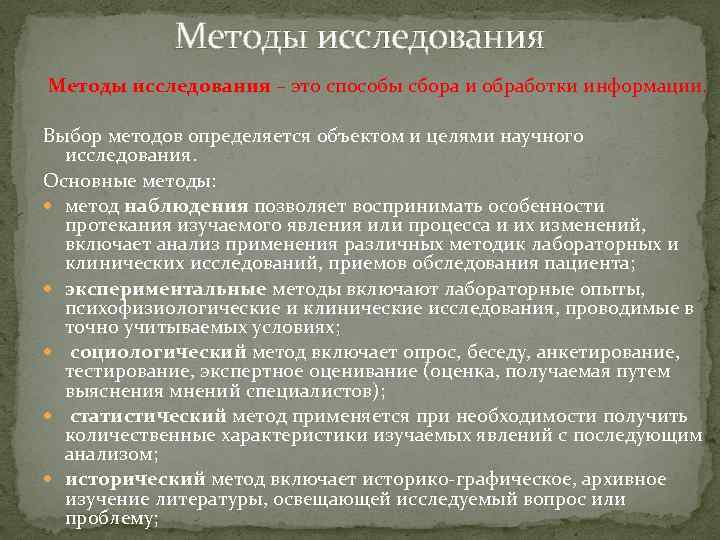 Research methods are ways of collecting and processing information. The choice of methods is determined by the object and goals of scientific research. Basic methods: the observation method allows one to perceive the peculiarities of the course of the studied phenomenon or process and their changes, includes an analysis of the use of various methods of laboratory and clinical research, methods of examining a patient; experimental methods include laboratory experiments, psychophysiological and clinical studies conducted under precisely accounted conditions; the sociological method includes a survey, conversation, questioning, testing, expert assessment (an assessment obtained by asking the opinions of specialists); the statistical method is used when it is necessary to obtain quantitative characteristics of the studied phenomena with subsequent analysis; the historical method includes the historical-graphic, archival study of literature covering the issue or problem under study;
Research methods are ways of collecting and processing information. The choice of methods is determined by the object and goals of scientific research. Basic methods: the observation method allows one to perceive the peculiarities of the course of the studied phenomenon or process and their changes, includes an analysis of the use of various methods of laboratory and clinical research, methods of examining a patient; experimental methods include laboratory experiments, psychophysiological and clinical studies conducted under precisely accounted conditions; the sociological method includes a survey, conversation, questioning, testing, expert assessment (an assessment obtained by asking the opinions of specialists); the statistical method is used when it is necessary to obtain quantitative characteristics of the studied phenomena with subsequent analysis; the historical method includes the historical-graphic, archival study of literature covering the issue or problem under study;
 Conclusions and Practical Recommendations Derived from the logic of the research; 2. Associated with the purpose of the work and the tasks set, the solution of which led to the formulation of conclusions; 3. A conclusion must be formulated for each task; 4. Recommendations are aimed at improving the process, activities, indicators, etc. 1.
Conclusions and Practical Recommendations Derived from the logic of the research; 2. Associated with the purpose of the work and the tasks set, the solution of which led to the formulation of conclusions; 3. A conclusion must be formulated for each task; 4. Recommendations are aimed at improving the process, activities, indicators, etc. 1.
 Conclusions 1. follow from the tasks 2. are formalized in the conclusion. Tasks 1. Analyze the regulatory documents governing the tactics of a paramedic during CPR. Conclusions 1. Analysis of the literature and normative documentation regulating the tactics of a paramedic during cardiopulmonary resuscitation has revealed that over the past five years there have been significant changes in the algorithm of cardiopulmonary resuscitation. Namely: The algorithm for the diagnosis of clinical death has been changed, which allows the most accurate and quick diagnosis, without wasting time trying to detect respiratory arrest with the help of a mirror, movement of a piece of thread, etc.; Methods of artificial ventilation of the lungs such as "mouth-to-nose" are not used, since its ineffectiveness has been proven and "from the mouth into the tracheostomy tube" because of the impossibility of observing hygiene standards when using this method; Simplified post-mortem support activities for all rescuers, whether they are qualified healthcare providers or non-professionals. This, accordingly, will reduce the mortality rate and the number of cases of disability as consequences of disruption of the brain after circulatory arrest.
Conclusions 1. follow from the tasks 2. are formalized in the conclusion. Tasks 1. Analyze the regulatory documents governing the tactics of a paramedic during CPR. Conclusions 1. Analysis of the literature and normative documentation regulating the tactics of a paramedic during cardiopulmonary resuscitation has revealed that over the past five years there have been significant changes in the algorithm of cardiopulmonary resuscitation. Namely: The algorithm for the diagnosis of clinical death has been changed, which allows the most accurate and quick diagnosis, without wasting time trying to detect respiratory arrest with the help of a mirror, movement of a piece of thread, etc.; Methods of artificial ventilation of the lungs such as "mouth-to-nose" are not used, since its ineffectiveness has been proven and "from the mouth into the tracheostomy tube" because of the impossibility of observing hygiene standards when using this method; Simplified post-mortem support activities for all rescuers, whether they are qualified healthcare providers or non-professionals. This, accordingly, will reduce the mortality rate and the number of cases of disability as consequences of disruption of the brain after circulatory arrest.
 Conclusion In the conclusion, the theoretical and practical results and judgments reached by the student as a result of the research are consistently stated. They should be concise, clear, giving a complete understanding of the content, relevance, validity and effectiveness of the work. The results (conclusions) of the research must correspond to the set goals and objectives.
Conclusion In the conclusion, the theoretical and practical results and judgments reached by the student as a result of the research are consistently stated. They should be concise, clear, giving a complete understanding of the content, relevance, validity and effectiveness of the work. The results (conclusions) of the research must correspond to the set goals and objectives.
 An example of a conclusion. Conclusion. Late cardiopulmonary resuscitation significantly reduces the chances of a full recovery of the body's vital functions. So, if resuscitation measures were started later than 10 minutes after cardiac arrest, then in the vast majority of cases, full restoration of the functions of the central nervous system is impossible. Surviving patients will have more or less pronounced neurological symptoms associated with damage to the cerebral cortex. If the provision of cardiopulmonary resuscitation began 15 minutes after the onset of clinical death, then in most cases there is complete death of the cerebral cortex, leading to social death of a person. In this case, it is possible to return only the autonomic functions of the body (independent respiration, nutrition, etc.), as a person dies. In 20 minutes after cardiac arrest, complete brain death usually occurs when even autonomic functions cannot be restored. Now complete brain death is legally equal to the death of a person, although the life of the body can still be maintained for some time with the help of modern medical equipment and pharmaceuticals. Thus, the following results can be summed up: 1. Analysis of the literature and normative documents regulating the tactics of a paramedic during cardiopulmonary resuscitation revealed that over the past five years there have been significant changes in the algorithm for cardiopulmonary resuscitation. Namely: The algorithm for the diagnosis of clinical death has been changed, which allows the most accurate and quick diagnosis, without wasting time trying to detect respiratory arrest using a mirror, movement of a piece of thread, etc.; Methods of artificial lung ventilation such as "mouth-to-nose" are not used, since its ineffectiveness has been proven and "from the mouth into the tracheostomy tube" due to the impossibility of observing hygiene standards when using this method; Simplified post-clinical death support activities for all resuscitators, whether they are qualified healthcare providers or non-professionals. This, accordingly, will reduce the mortality rate and the number of cases of disability as a consequence of the disruption of the brain after circulatory arrest. 2. As a result of the analysis of the factors affecting the threat of terminal conditions, it follows that their risk of development in the analyzed area is low and the maximum possible work is carried out to further reduce it, but at the same time, to provide the most complete and timely emergency care, it is necessary to improve the equipment of the Medyaginsky FAP, replace CPR instructions, conduct health education among the population regarding changes in CPR standards, since it is the possession of CPR techniques for as many residents as possible that will allow timely assistance to the victim and, therefore, increase the chances of successful completion of resuscitation actions. 3. An analysis of the effectiveness of cardiopulmonary resuscitation carried out by the teams of the emergency medical service in Yaroslavl showed that the number of deaths in 2014 decreased compared to 2013 by 0.02%, which indicates the effectiveness of CPR due to the rapid timely arrival of paramedics and specialized teams, and also their full equipment, the introduction of a new CPR protocol from 2010. 4. Having analyzed the literature and normative documentation regulating the tactics of a paramedic during cardiopulmonary resuscitation, having studied the prevalence of factors affecting the threat of terminal conditions and the statistics of EMC, the following suggestions for techniques and means that increase the efficiency of a paramedic's cardiopulmonary resuscitation: control the professional knowledge and skills of paramedics in CPR; control the equipment of FAPs and other prehospital services with the necessary set of resuscitation equipment; regularly study; control the knowledge of orders; update manuals and instructions in a timely manner. All this will increase the survival rate of patients until the arrival of specialized ambulance teams.
An example of a conclusion. Conclusion. Late cardiopulmonary resuscitation significantly reduces the chances of a full recovery of the body's vital functions. So, if resuscitation measures were started later than 10 minutes after cardiac arrest, then in the vast majority of cases, full restoration of the functions of the central nervous system is impossible. Surviving patients will have more or less pronounced neurological symptoms associated with damage to the cerebral cortex. If the provision of cardiopulmonary resuscitation began 15 minutes after the onset of clinical death, then in most cases there is complete death of the cerebral cortex, leading to social death of a person. In this case, it is possible to return only the autonomic functions of the body (independent respiration, nutrition, etc.), as a person dies. In 20 minutes after cardiac arrest, complete brain death usually occurs when even autonomic functions cannot be restored. Now complete brain death is legally equal to the death of a person, although the life of the body can still be maintained for some time with the help of modern medical equipment and pharmaceuticals. Thus, the following results can be summed up: 1. Analysis of the literature and normative documents regulating the tactics of a paramedic during cardiopulmonary resuscitation revealed that over the past five years there have been significant changes in the algorithm for cardiopulmonary resuscitation. Namely: The algorithm for the diagnosis of clinical death has been changed, which allows the most accurate and quick diagnosis, without wasting time trying to detect respiratory arrest using a mirror, movement of a piece of thread, etc.; Methods of artificial lung ventilation such as "mouth-to-nose" are not used, since its ineffectiveness has been proven and "from the mouth into the tracheostomy tube" due to the impossibility of observing hygiene standards when using this method; Simplified post-clinical death support activities for all resuscitators, whether they are qualified healthcare providers or non-professionals. This, accordingly, will reduce the mortality rate and the number of cases of disability as a consequence of the disruption of the brain after circulatory arrest. 2. As a result of the analysis of the factors affecting the threat of terminal conditions, it follows that their risk of development in the analyzed area is low and the maximum possible work is carried out to further reduce it, but at the same time, to provide the most complete and timely emergency care, it is necessary to improve the equipment of the Medyaginsky FAP, replace CPR instructions, conduct health education among the population regarding changes in CPR standards, since it is the possession of CPR techniques for as many residents as possible that will allow timely assistance to the victim and, therefore, increase the chances of successful completion of resuscitation actions. 3. An analysis of the effectiveness of cardiopulmonary resuscitation carried out by the teams of the emergency medical service in Yaroslavl showed that the number of deaths in 2014 decreased compared to 2013 by 0.02%, which indicates the effectiveness of CPR due to the rapid timely arrival of paramedics and specialized teams, and also their full equipment, the introduction of a new CPR protocol from 2010. 4. Having analyzed the literature and normative documentation regulating the tactics of a paramedic during cardiopulmonary resuscitation, having studied the prevalence of factors affecting the threat of terminal conditions and the statistics of EMC, the following suggestions for techniques and means that increase the efficiency of a paramedic's cardiopulmonary resuscitation: control the professional knowledge and skills of paramedics in CPR; control the equipment of FAPs and other prehospital services with the necessary set of resuscitation equipment; regularly study; control the knowledge of orders; update manuals and instructions in a timely manner. All this will increase the survival rate of patients until the arrival of specialized ambulance teams.
 Requirements for the list of references Normative legal documents and sources: orders federal, regional, Procedures and standards, San. Pins, GOSTs Monographs Collections Printed articles Internet editions Uniform alphabetical numbering Full compliance with the text of the work
Requirements for the list of references Normative legal documents and sources: orders federal, regional, Procedures and standards, San. Pins, GOSTs Monographs Collections Printed articles Internet editions Uniform alphabetical numbering Full compliance with the text of the work
 Requirements for the paperwork When compiling this manual, the following GOSTs were used: GOST 2. 105 - 95. ESKD. "General requirements for text documents" (updated on 13.01.2010) GOST 7. 32 - 2001 "Report on research work. Structure and design rules "GOST R 6. 30 - 2003" Unified documentation system. Unified system of organizational and administrative documentation. Requirements for paperwork. "GOST 7. 1 - 2003" Bibliographic record. Bibliographic description. General requirements and rules for compilation "GOST 7. 12 - 77" Abbreviation of Russian words and phrases in the bibliographic description "GOST 7. 11- 78" Abbreviations of words and phrases in foreign languages \u200b\u200bin the bibliographic description "GOST 7. 80 - 2000" Bibliographic record. Title. General requirements and rules for compilation "GOST 7. 82 - 2001" Bibliographic description of electronic resources: general requirements and rules for compilation "GOST 7. 0. 5 - 2008" Bibliographic reference. General requirements and rules of drawing up ".
Requirements for the paperwork When compiling this manual, the following GOSTs were used: GOST 2. 105 - 95. ESKD. "General requirements for text documents" (updated on 13.01.2010) GOST 7. 32 - 2001 "Report on research work. Structure and design rules "GOST R 6. 30 - 2003" Unified documentation system. Unified system of organizational and administrative documentation. Requirements for paperwork. "GOST 7. 1 - 2003" Bibliographic record. Bibliographic description. General requirements and rules for compilation "GOST 7. 12 - 77" Abbreviation of Russian words and phrases in the bibliographic description "GOST 7. 11- 78" Abbreviations of words and phrases in foreign languages \u200b\u200bin the bibliographic description "GOST 7. 80 - 2000" Bibliographic record. Title. General requirements and rules for compilation "GOST 7. 82 - 2001" Bibliographic description of electronic resources: general requirements and rules for compilation "GOST 7. 0. 5 - 2008" Bibliographic reference. General requirements and rules of drawing up ".
 No. Object of unification of final qualifying works Unification parameters Requirements for design 1 Paper sheet size A 4 2 Font size 14 points 3 Font name Times New Roman 4 Line spacing One and a half 5 Lines per page 28 30 lines (1800 printed characters) 6 Paragraph 1, 25 cm (5 characters) 7 Margins (mm) Left, top and bottom - 20, right - 10 8 Total volume without attachments 50 60 typewritten pages 9 Introduction volume 2 4 typewritten pages 10 Main part 40 50 pages of typewritten text 11 Volume of the conclusion 3 5 pages of typewritten text (approximately equal to the volume of the introduction) 12 Numbering of pages Through, at the bottom of the sheet, in the middle. The page number does not appear on the title page 13 Sequence Title page. The task for the execution of the graduation reduction of the structural qualification work. Content. Introduction. parts of work The main part. Conclusion. Glossary. List of sources used. List of abbreviations. Applications 14 Structural design Each structural part begins with a new part of the page work. The names are given from a paragraph with an uppercase (capital letter). The period at the end of the name is not put 15 Structure of the main part 2 3 chapters, commensurate in size 16 Availability of a glossary 15 20 concepts 17 Composition of the list of used 30 50 bibliographic descriptions of documentary sources and literary sources 18 Availability of appendices Required 19 Content design Content (table of contents) includes headings (tables of contents) of all sections, chapters, paragraphs, glossary, annexes with indication of the beginning pages of each part
No. Object of unification of final qualifying works Unification parameters Requirements for design 1 Paper sheet size A 4 2 Font size 14 points 3 Font name Times New Roman 4 Line spacing One and a half 5 Lines per page 28 30 lines (1800 printed characters) 6 Paragraph 1, 25 cm (5 characters) 7 Margins (mm) Left, top and bottom - 20, right - 10 8 Total volume without attachments 50 60 typewritten pages 9 Introduction volume 2 4 typewritten pages 10 Main part 40 50 pages of typewritten text 11 Volume of the conclusion 3 5 pages of typewritten text (approximately equal to the volume of the introduction) 12 Numbering of pages Through, at the bottom of the sheet, in the middle. The page number does not appear on the title page 13 Sequence Title page. The task for the execution of the graduation reduction of the structural qualification work. Content. Introduction. parts of work The main part. Conclusion. Glossary. List of sources used. List of abbreviations. Applications 14 Structural design Each structural part begins with a new part of the page work. The names are given from a paragraph with an uppercase (capital letter). The period at the end of the name is not put 15 Structure of the main part 2 3 chapters, commensurate in size 16 Availability of a glossary 15 20 concepts 17 Composition of the list of used 30 50 bibliographic descriptions of documentary sources and literary sources 18 Availability of appendices Required 19 Content design Content (table of contents) includes headings (tables of contents) of all sections, chapters, paragraphs, glossary, annexes with indication of the beginning pages of each part
 Example of table design Table 1 Comparative characteristics of the equipment of vehicles of various classes Recommended equipment for ambulance teams type A type B type C MEDICAL KITS Infusion set for ambulance NISP-05 1 Trauma kit for ambulance NIT-01 1 Obstetric kit for ambulance NISP-06 1 1 Resuscitation kit for ambulance IISP 1 1
Example of table design Table 1 Comparative characteristics of the equipment of vehicles of various classes Recommended equipment for ambulance teams type A type B type C MEDICAL KITS Infusion set for ambulance NISP-05 1 Trauma kit for ambulance NIT-01 1 Obstetric kit for ambulance NISP-06 1 1 Resuscitation kit for ambulance IISP 1 1
 Design of attachments Material supplementing the main part of the CD is drawn up in the form of attachments. They are designated in capital letters, with the exception of E, Z, Y, O, H, L, S, b Each attachment starts from a new page. They have common page numbering with the main part of the document
Design of attachments Material supplementing the main part of the CD is drawn up in the form of attachments. They are designated in capital letters, with the exception of E, Z, Y, O, H, L, S, b Each attachment starts from a new page. They have common page numbering with the main part of the document
 Design of applications In the text of the CD should For example: there should be links to all The main manifestations of the application of changes in the bone References to the applications of the system in cirrhosis in the text of the CD should be organized in strictly changes of the fingers in the numerical order in the form of "drumsticks", nails - in the form of " watch glasses "(Appendix B).
Design of applications In the text of the CD should For example: there should be links to all The main manifestations of the application of changes in the bone References to the applications of the system in cirrhosis in the text of the CD should be organized in strictly changes of the fingers in the numerical order in the form of "drumsticks", nails - in the form of " watch glasses "(Appendix B).
 Tactical mistakes Errors in the style of presentation Basic requirements for the style of presentation The thesis / course work should be presented in a laconic, clear, literate language. Proposals dedicated to the presentation of any specific thought, ideas should be combined into a separate paragraph. The presentation and arrangement of the questions and sections of the thesis considered in the text part should be consistent and logical. To display numerical data, analysis results, generalize indicators, identify the relationships of the studied quantities, you should use illustrations (photographs, diagrams, diagrams, tables, etc.). It is recommended to present the material in the diploma in your own words, avoiding verbatim rewriting from literary sources. Arbitrary abbreviation of words is also not allowed. Quotations, data, figures, tables, statements of views of other authors borrowed from the literature should be provided with links to relevant sources. When writing the text of the thesis, the general tone of the presentation of the material should be calm, and the statements should be reasoned. The material should be presented in the first person plural, for example: we analyze, design, choose. You can also use an indefinite form, for example: should be accepted, considered appropriate, etc. In all work, it is necessary to use a single terminology. If the term has synonyms, then you should choose one of them. Usually, a multiple-word, wordy term is replaced by an abbreviation. An important condition for preventing errors is a preliminary reading of the diploma materials by the head and the consultant, who note the mistakes made by the student and indicate what needs to be shortened, supplemented, explained. The student should write down and take into account the critical remarks. It is recommended to show the work to specialists and practitioners in the organization on the basis of which it was written.
Tactical mistakes Errors in the style of presentation Basic requirements for the style of presentation The thesis / course work should be presented in a laconic, clear, literate language. Proposals dedicated to the presentation of any specific thought, ideas should be combined into a separate paragraph. The presentation and arrangement of the questions and sections of the thesis considered in the text part should be consistent and logical. To display numerical data, analysis results, generalize indicators, identify the relationships of the studied quantities, you should use illustrations (photographs, diagrams, diagrams, tables, etc.). It is recommended to present the material in the diploma in your own words, avoiding verbatim rewriting from literary sources. Arbitrary abbreviation of words is also not allowed. Quotations, data, figures, tables, statements of views of other authors borrowed from the literature should be provided with links to relevant sources. When writing the text of the thesis, the general tone of the presentation of the material should be calm, and the statements should be reasoned. The material should be presented in the first person plural, for example: we analyze, design, choose. You can also use an indefinite form, for example: should be accepted, considered appropriate, etc. In all work, it is necessary to use a single terminology. If the term has synonyms, then you should choose one of them. Usually, a multiple-word, wordy term is replaced by an abbreviation. An important condition for preventing errors is a preliminary reading of the diploma materials by the head and the consultant, who note the mistakes made by the student and indicate what needs to be shortened, supplemented, explained. The student should write down and take into account the critical remarks. It is recommended to show the work to specialists and practitioners in the organization on the basis of which it was written.
 work Scheme of the report on the defense of the final qualifying work 1. Address: Dear chairman and members of the State Attestation Commission! Your attention is invited to the final qualifying work on the topic ... 2. In 2 - 3 sentences, a characteristic of the relevance of the topic is given. 3. A brief review of literary sources on the selected problem (degree of elaboration of the problem) is given. 4. The purpose of the final qualifying work - the purpose of the work is formulated. 5. Tasks are formulated, titles of chapters are given. In this case, the formulation must contain verbs of the type - study, consider, reveal, formulate, analyze, define, etc. 6. From each chapter, conclusions or formulations are used that characterize the results. Here you can show posters / slides When showing slides, do not read the text shown on them. You just need to describe the image in one or two phrases. If charts are shown, then they must be named and the trends observed on the charts must be stated. When demonstrating diagrams, pay attention to the designation of segments, columns, etc. The graphic material should be visual and understandable from the outside. Text accompanying charts and bar charts should only reflect specific conclusions. The volume of this part of the report should not exceed 1, 52 pages of printed text. 7. As a result of the research, the following conclusions were made: (the main conclusions drawn in the conclusion are formulated). 8. Based on the conclusions, the following proposals were made: (proposals are listed). Note. The seventh and eighth parts of the report should not exceed 1 page of printed text in total. In total, the entire report with a timing of 10 12 minutes (with demo material) fits into 3 4 pages of printed text with line spacing of 1, 0 and font (14 points).
work Scheme of the report on the defense of the final qualifying work 1. Address: Dear chairman and members of the State Attestation Commission! Your attention is invited to the final qualifying work on the topic ... 2. In 2 - 3 sentences, a characteristic of the relevance of the topic is given. 3. A brief review of literary sources on the selected problem (degree of elaboration of the problem) is given. 4. The purpose of the final qualifying work - the purpose of the work is formulated. 5. Tasks are formulated, titles of chapters are given. In this case, the formulation must contain verbs of the type - study, consider, reveal, formulate, analyze, define, etc. 6. From each chapter, conclusions or formulations are used that characterize the results. Here you can show posters / slides When showing slides, do not read the text shown on them. You just need to describe the image in one or two phrases. If charts are shown, then they must be named and the trends observed on the charts must be stated. When demonstrating diagrams, pay attention to the designation of segments, columns, etc. The graphic material should be visual and understandable from the outside. Text accompanying charts and bar charts should only reflect specific conclusions. The volume of this part of the report should not exceed 1, 52 pages of printed text. 7. As a result of the research, the following conclusions were made: (the main conclusions drawn in the conclusion are formulated). 8. Based on the conclusions, the following proposals were made: (proposals are listed). Note. The seventh and eighth parts of the report should not exceed 1 page of printed text in total. In total, the entire report with a timing of 10 12 minutes (with demo material) fits into 3 4 pages of printed text with line spacing of 1, 0 and font (14 points).
 The order of the completion of the WRC by students Period October November December January - February March April - May June Stages of the WRC implementation The choice of the problem and the formulation of the topic. Drawing up an indicative research plan. Selection of literature on the topic. Working with sources. Determination of the main methodological characteristics of the work: the allocation of the object and the subject of research, the formulation of goals, hypotheses, research objectives, the choice of research methods. Working with sources. Writing the theoretical part of the FQP. Development of the practical part of the work. Practical work, analysis of indicators. Work with sources, systematization of material, editing of theoretical paragraphs of the work. The final formulation of the research topic. Conducting the practical part of the work. Description of this stage of work. Analysis of the results of the practical part of the work. Description of the final stage of work. Generalization of research materials on the topic of work. WRC pre-protection. Final design of the work: writing conclusions by chapters, writing an introduction and conclusion, drawing up the final version of the bibliography, designing annexes, title page, content sheet, layout and binding of the thesis. Checking the work by the supervisor. Reviewing the work. Execution of procedural points. WRC protection.
The order of the completion of the WRC by students Period October November December January - February March April - May June Stages of the WRC implementation The choice of the problem and the formulation of the topic. Drawing up an indicative research plan. Selection of literature on the topic. Working with sources. Determination of the main methodological characteristics of the work: the allocation of the object and the subject of research, the formulation of goals, hypotheses, research objectives, the choice of research methods. Working with sources. Writing the theoretical part of the FQP. Development of the practical part of the work. Practical work, analysis of indicators. Work with sources, systematization of material, editing of theoretical paragraphs of the work. The final formulation of the research topic. Conducting the practical part of the work. Description of this stage of work. Analysis of the results of the practical part of the work. Description of the final stage of work. Generalization of research materials on the topic of work. WRC pre-protection. Final design of the work: writing conclusions by chapters, writing an introduction and conclusion, drawing up the final version of the bibliography, designing annexes, title page, content sheet, layout and binding of the thesis. Checking the work by the supervisor. Reviewing the work. Execution of procedural points. WRC protection.

When we seek medical help, we usually think that we are going "to the doctor." Although, in fact, first of all we get to other specialists - paramedics. As a rule, they are the first to assess our condition, provide emergency assistance and refer to more narrow specialists. What is this profession, how does it differ from others?
Few facts about the paramedic profession
The word "feldscher" in translation from German means "field barber". The first paramedics appeared in Germany in the Middle Ages - they provided emergency assistance to the wounded during battles. Over time, their functions practically did not change: for many centuries, paramedics were assigned the responsibility of providing first aid, emergency diagnostics, and carrying out the necessary medical procedures.
However, there is no such profession in the European Union now. It has survived only in Poland, and in very small quantities and with a significant reduction in functionality.
On the other hand, in the USA and Canada, the Physician assistant is a respected and responsible profession, whose representatives perform various functions, including medical ones.
Paramedic's Day in Russia
In Russia, the appearance of the first paramedic workers is associated with the creation in 1818 of a kind of analogue of the "Ambulance" - a special service that could provide first aid at home. Paramedics celebrate their professional holiday on February 21. Unfortunately, this day has no official status.
Paramedic profession code according to OKPDTR
In the All-Russian Classifier of Workers' Professions, Employee Positions and Wage Grades (OKPDTR), the paramedic profession is designated by the code 27328.
What is the difference between a paramedic and a doctor?

A paramedic is a specialist who has received secondary specialized medical education.
In the medical hierarchy, it sits between the doctor and the nurse. He has the right to conduct examinations and establish a diagnosis, conduct self-treatment or refer a patient to a specialist doctor.
Unlike a nurse, a paramedic is qualified to diagnose and treat diseases. The nurse does not prescribe treatment: she provides care and looks after the sick.
There are fewer differences in the activities of a paramedic and a doctor. A paramedic in many cases is able to replace a doctor, but the level of professional knowledge of a doctor is higher, therefore, a paramedic works under the supervision of a doctor.
Where are paramedics in demand?
The role of a paramedic is especially important in places remote from large medical institutions. In villages, for example, the work of a paramedic is practically no different from that of a district doctor. And the institution where he works is called the feldsher-midwife point (FAP). Here, a paramedic often performs the functions of a therapist, a nurse, and even an obstetrician.
Paramedics also work at ambulances, medical centers at airports, railway and bus stations, military units, and health centers of large enterprises.
In large medical institutions, where there are no problems with personnel, paramedics help doctors.
Paramedic specialization

Paramedics are in demand in a wide variety of areas of medical services. The main specialties of a paramedic are:
Feldsher-obstetrician. Monitors pregnant women, helps the doctor to conduct examinations and maintains documentation, if necessary, participates in childbirth.
Children's paramedic. Conducts examination of newborns, supervises the condition of children of all age categories.
Paramedic laboratory assistant. Collects material for analyzes. Has the right to independently conduct some research.
Sanitary paramedic. Responsible for the sanitary condition of children's institutions, hospitals, beauty salons, grocery stores, etc.
Ambulance paramedic. He works on calls, provides emergency assistance, decides on hospitalization of patients. Performs the functions of a doctor's assistant, but can also work independently, leading a team.
Military paramedic. Checks the condition of military personnel and conscripts; assists in treatment during military operations in the field and in the hospital. As a rule, such specialists are trained by military medical academies.
Local paramedic. In fact, he performs the duties of a therapist in a FAP or in a medical unit at a large enterprise, carries out treatment and prevention. At enterprises, he is also responsible for the observance of working conditions.
Where can you learn to be a paramedic?
To work as a paramedic, secondary specialized education is sufficient. You can get it at any medical college or university.
The direction of training is suitable for any of the traditionally offered:
"General Medicine";
"Medical and Preventive Business";
"Nursing business".
You can apply both after the 9th and after the 11th grade. The exception is the specialty "General Medicine" - here they are accepted only with a certificate of secondary education, that is, after the 11th grade.
The term of study at the college on the basis of 11 classes is: 2 years 10 months (for the specialty "General Medicine" - 3 years 10 months). The term of study for those who enter after the 9th grade is increased by 1 year (3 years 10 months).
Despite the fact that the position of a medical assistant does not provide for compulsory higher education, some specialists working as medical assistants have higher medical education. This is often due to the fact that after university graduates find it easier to get a medical assistant position. As a rule, in the future, such a specialist manages to quickly rise to the level of a doctor.
Specialists with higher education are also predominantly moving up the career ladder.
As with other medical specialties, a paramedic, in addition to a high school diploma, for.
Salary and career prospects
Since the specialty of a paramedic assumes versatile medical knowledge, the ability to carry out various procedures, this is a profession that is quite in demand in the labor market. But not the most profitable.
The average monthly salary of a paramedic depends on many factors: the level of the medical institution, its location, the length of service of the specialist, his qualifications.
The lowest wages are offered in rural FAPs, here it varies on average from 20 to 40 thousand rubles, but there are cases when a paramedic is offered lower salaries.
The highest is in prestigious private clinics, where the salary is set after an interview and can be comparable to that of a highly qualified doctor.
It should be remembered that now the country has a program of state support for health workers "Zemsky Feldsher", according to which feldshers who are ready to move to the countryside are provided with a lifting payment of 500 thousand rubles, which can be spent on improving their living conditions. At the same time, the health worker undertakes to work in rural areas for at least 5 years.
The career development of a paramedic is usually associated with further education at a university and obtaining a specialty as a doctor.
At the same time, even with a secondary education, a paramedic can count on career growth. To advance in the administrative line, you need at least five years of experience and completion of nursing management courses.
When working at paramedic points, it is possible to obtain the position of a manager.
Pros and cons of the profession
shorter training period compared to a doctor;
demand for specialists;
variety of fields of activity;
the opportunity to combine work in medical institutions with part-time work in private organizations (beauty salons, swimming pools, etc.);
high social significance of the profession.
a wide range of responsibilities;
physical activity and great responsibility;
irregular working hours;
demand, mainly in small medical institutions.
FELDSHER
Man has the right to be bad an artist or a carpenter,
but does not havethe right to be a bad doctor.
V. Ya. Danilevsky
Profession "paramedic "
first appeared in Germany; the term "feldscher" itself is translated from German as "field barber", as in the Middle Ages they called a person who provided medical care directly on the battlefield during wars. Today, a paramedic is an assistant or assistant to a doctor in urban and regional medical institutions, and in rural medical posts he performs the functions of both a doctor and a manager. The profession of a medical assistant is very responsible and important, as it combines considerable medical knowledge with unique practical skills.
The following specializations are distinguished in this profession:
Paramedic laboratory assistant;
Ambulance paramedic;
Feldsher-obstetrician;
Sanitary paramedic;
Military paramedic.
With all the variety of specialties of this profession in educational organizations, you can get a general medical assistant education with the qualification of a "medical assistant", however, the content of a specialist's professional activity will be determined by the specifics of the place of work.
Professionally important qualities:
good operational and long-term memory;
organizational skills;
the ability to concentrate and distribute attention; 
good hand-eye coordination;
the ability to act effectively in a crisis situation;
logical and analytical thinking;
communication skills;
benevolence;
self-control;
a responsibility;
tact;
accuracy;
stress resistance;
physical endurance;
neuropsychic stability.
Medical restrictions:
Reduced level of vision and hearing;
cardiovascular diseases;
neuropsychiatric diseases;
allergy to drugs;
disorders of the musculoskeletal system;
chronic infectious diseases.
Paramedic is a specialist with a secondary medical education. Provides first pre-medical, urgent and emergency medical care to the sick and injured. Working in the ambulance team, he is a doctor's assistant and works under his supervision. Provides independent inpatient, outpatient and home care, performing the functions of a doctor in rural health centers; conducts measures to prevent and reduce morbidity, early detection of diseases; assists in childbirth; conducts various analyzes; develops treatment-and-prophylactic and sanitary-hygienic measures and participates in their implementation; performs medical appointments; supervises the actions of junior medical personnel. The range of responsibilities depends largely on the place of work.
Educational organizations of Omsk and Omsk region:
Medical College of the Omsk Region;
Omsk Medical School of Railway Transport (OmGUPS);
Omsk State Medical Academy of the Ministry of Health of the Russian Federation.
Professional activity
Most of the college graduates go to the Emergency Medical Service. Only doctors and paramedics are allowed to work here. There are no nurses in the ambulance, and the paramedic works in the same team with the doctor or in a special paramedic team. In both cases, the paramedic must have a fairly broad medical knowledge, be able to make decisions correctly and quickly. He can work in health centers, hospitals, clinics, dispensaries, sanatoriums, maternity hospitals and other medical institutions.
Career
Paramedics are constantly in demand in the labor market. In the future, a paramedic can become the head of a health center, a senior paramedic. Higher medical education provides an opportunity for career growth.
Introduction
Thermal injuries (injuries) represent a serious medical, social and economic problem and occupy the third place in the structure of peacetime injuries.
This problem has especially increased in connection with man-made accidents, increased production, the development of vehicles, increased urbanization of the population and an increase in natural disasters.
More than 600 thousand cases of burn injuries are registered in Russia annually. At the same time, about 70% of patients receive limited area and shallow burns. They receive help mainly on an outpatient basis.
According to Russian authors, mortality from burns in Russia as a whole ranges from 2.3% to 3.6%. Of the 180-200 thousand victims hospitalized in all medical institutions in Russia, 8-10 thousand people die annually. At the same time, 85-90% are people of working age and children. And out of the number of survivors, 12-15 thousand people need long-term rehabilitation.
Of the burned, hospitalized in hospitals, 60-80% of patients also have superficial and borderline II-IIIA degree burns that do not require surgical treatment. However, such burns largely determine the severity of the injury and its prognosis.
Electric burns in frequency among burns from other causes account for only 2 - 3%, but they often cause disability and, in some cases, death.
Rehabilitation is the restoration of health, functional state and working capacity, impaired by diseases, injuries or physical, chemical and social factors. The goal of rehabilitation is the effective and early return of sick and disabled people to everyday and work processes, into society, and the restoration of a person's personal properties. The World Health Organization (WHO) gives a very close definition of rehabilitation: "Rehabilitation is a set of measures designed to provide people with impaired functions as a result of diseases, injuries, birth defects, adaptation to new living conditions in the society in which they live."
According to WHO, rehabilitation is a process aimed at comprehensive assistance to sick and disabled people in order to achieve the maximum possible physical, mental, professional, social and economic usefulness in this disease.
Increasing the efficiency of the paramedic's work based on the model of organizing medical care for patients with thermal injuries allows realizing these directions and achieving an increase in the quality of life after injury. The aim of this course work is to analyze the role of a paramedic in carrying out rehabilitation measures for patients with thermal injuries to improve their quality of life.
To achieve the goal set in the course work, the following tasks were identified:
Consider the anatomy of tissue exposed to thermal factors.
List the most common causes of thermal damage.
Classify thermal damage.
Describe the methods of treatment and rehabilitation for thermal injuries.
Determine the activities of the paramedic during the
Analyze the effectiveness of the rehabilitation performed.
The object of research is thermal damage.
The coursework consists of two chapters. The first chapter examines the anatomy, clinical manifestations, methods of treatment and rehabilitation for thermal injuries.
The second chapter, which is a practical part, provides a statistical analysis of the cases of patients' appeals to the FAP paramedic associated with thermal injuries, as well as paramedic activities during rehabilitation measures.
1.Treatment and rehabilitation for thermal injuries
.1 Anatomy: human skin, eyes, oral cavity
The skin is formed by three layers of tissues: the outer layer is the epidermis, the dermis is located under it, the deep layer is the subcutaneous tissue. The epidermis is a type of epithelial tissue. The outer layer of the epidermis is dead keratinized cells. They constantly peel off: every minute you lose about 50 thousand of these horny scales. However, the thickness of the epidermis does not decrease.
The upper layer of the epidermis is constantly renewed by the cells of the lower layer, which are cubic in shape and are constantly dividing. Some cells remain in the lower layer, while others form the upper layer. These cells lose their ability to divide, flatten, accumulate the protein keratin, and, as a result, they become keratinized, dead and exfoliated. In the lower layer of the epidermis, new cells are constantly being produced. So in 10-30 days it is completely renewed. Typically the epidermis is 0.03-1.5 mm thick. But in areas of the body experiencing strong friction (palms, feet), it is several times thicker.
1.2 Derma
The intercellular substance of the connective tissue, which forms the dermis, contains collagen and elastic fibers. Thanks to them, the skin is elastic and easily stretched: pull it back on the back of your hand and release it - it will immediately return to its original state.
The thickness of the dermis is 0.5-5 mm, it is thick on the back, shoulders, hips. The dermis protrudes into the epidermis with many papillae, which lift the epidermis to form ridges and ridges. Their drawing is different for each person. In the dermis there are blood and lymphatic capillaries, muscle and nerve fibers, nerve endings, pigment cells, sweat and sebaceous glands, hair follicles. Skin glands are endocrine glands that secrete secretions onto the surface of the skin. The sweat gland looks like a tube with a diameter of 0.3-0.4 mm, twisted into a ball. One end of it is connected to the time in the epidermis. In humans, unlike other mammals, sweat glands are located on the entire surface of the body, but most of them are on the palms, feet, and armpits. The secretion of the sweat glands is sweat, which is formed from the intercellular fluid. It consists of 98% water, the rest is salts, urea and other metabolic products dissolved in it.
Unlike sweat glands, the sebaceous glands are branched, and their ducts open into the hair follicle. Most of the sebaceous glands are located on the head, face, and upper back. their secret contains fatty substances. They reach the hair and skin surface and soften it. The waterproof layer formed by these substances protects the skin from dust and microorganisms and also prevents it from drying out. The sebaceous glands secrete about 20 g of secretion per day.
Subcutaneous tissue is the lower layer of the skin formed by adipose tissue 3-10 mm thick. The subcutaneous tissue acts as a shock absorber that dampens mechanical stress on the body surface. No wonder a thick layer of this tissue is found on the buttocks and soles - they are constantly under great pressure. Adipose tissue is a good heat insulator, so thin ones usually freeze more than fat ones.
Derivatives of the epidermis perform an additional protective function, are hair and nails. Hair covers almost the entire surface of the skin, with the exception of the palms, soles, lateral surfaces of the fingers. On average, about 100 thousand hairs grow on a person's head, and although a person loses 75-100 of them daily, their number is normally restored.
In the hair, a shaft protruding above the skin and a root located in the dermis are distinguished. The root is located in the hair follicle and ends with a thickening - the hair follicle. The base of the follicle is connected to the smooth muscle, when the contraction of which the hair rises. The hair follicle is made up of epithelial cells that divide to grow hair. Moving to the surface of the skin, these cells are filled with keratin and keratinized. In a month, the hair grows by about 1 cm. The cells of the hair follicle are capable of dividing within 2-4 years, then the hair growth stops and it falls out. After a while, the hair follicle can restore its activity.
Hair color is determined by the amount of melanin pigment contained in its outer layer. With age, melanin synthesis decreases and hair turns gray.
The nail is a dense stratum corneum that lies on the nail bed. The bed is bounded from the sides by skin folds - nail ridges. The nail grows due to cell division of the root of the nail in the same way as hair grows.
1.3 Skin functions
The skin is one of the largest organs in the human body, its mass in an adult reaches 5 kg, and its area is 1.5-2 m2. And this is not surprising, because it is a shell that separates almost the entire human body from the external environment. The skin protects the internal organs from mechanical damage, from the penetration of various substances and microorganisms, from the harmful effects of ultraviolet radiation.
With the secretion of the sweat glands of the skin, water and certain metabolic products are released.
The skin also works as a sense organ. The sensation of touch, pressure, vibration, pain occurs due to the stimulation of the corresponding neurons, the nerve endings of which are contained in the skin. Thanks to the thermoreceptor neurons of the skin, you perceive changes in ambient temperature. The skin plays an important role in thermoregulation: almost 82% of the body's total heat transfer occurs through it.
Skin is a blood depot and storage of reserve substances. The branched network of its vessels can hold up to 1 liter of blood, and fat accumulates in the subcutaneous adipose tissue. The role of the skin in metabolism is unique: vitamin D is synthesized only in its cells under the influence of ultraviolet radiation.
1.4 Organ of vision
Our eye is a complex optical system whose main task is to transmit images to the optic nerve. The initially visible image passes through the cornea. There is the primary refraction of light. From there, through a round hole in the iris, called the pupil, it enters the lens. Since the lens is a biconvex lens, after passing through the vitreous, the visible image is reversed when it hits the retina. It is the signal of the inverted image that comes from the retina along the optic nerve to the brain. And the brain is for that and the brain is to turn the image back.
1.5 External structure
1.6 Eyelids
The eyelids (upper and lower) are covered on the outside by skin, from the inside by a mucous membrane (conjunctiva). In the thickness of the eyelids, there are cartilage, muscles (the circular muscle of the eye and the muscle that lifts the upper eyelid) and glands. The eyelid glands produce components of the eye tear, which normally wets the surface of the eye.
On the free edge of the eyelids, eyelashes grow, which perform a protective function, and the ducts of the glands open. The palpebral fissure is located between the edges of the eyelids. In the inner corner of the eye, on the upper and lower eyelids, there are lacrimal points - holes through which a tear flows through the nasolacrimal canal into the nasal cavity.
1.7 Shells of the eyeball
The human eyeball has 3 shells: outer, middle and inner.
The sclera occupies 4/5 of the fibrous membrane and consists of connective tissue, it is dense enough and the eye muscles are attached to it. The main function is protective, it provides a certain shape and tone of the eyeball. From the posterior pole of the eye in the sclera there is a place of exit of the optic nerve - the ethmoid plate. The cornea is 1/5 of the outer shell, it has a number of characteristics: transparency (absence of blood vessels), luster, sphericity and sensitivity. All these signs are characteristic of a healthy cornea. With diseases of the cornea, these signs change (opacity, loss of sensitivity, etc.). The cornea belongs to the optical system of the eye, it conducts and refracts light (its thickness in different sections ranges from 0.2 to 0.4 mm, and the refractive power of the cornea is approximately 40 diopters).
The middle (choroid) of the eye consists of the iris, the ciliary body and the choroid itself (choroid), which are located directly under the sclera. The middle membrane of the eye provides nutrition to the eyeball, participates in metabolic processes and the excretion of metabolic products of the eye tissues. The iris is the anterior part of the vascular tract of the eye, it is located behind the transparent cornea, in the center there is an adjustable round opening - the pupil. Thus, the iris in the structure of the human eye plays the role of a diaphragm, painted in a certain color. Human eye color is determined by the amount of melanin pigment in the iris (light blue to brown). This pigment protects the eyes from excess sunlight. The pupil diameter varies from 2 to 8 mm, depending on the illumination, nervous regulation or the action of medications. Normally, the pupil narrows in bright light and dilates in low light.
1.8 Most common causes of thermal damage
Burns are caused by exposure to high temperatures (thermal burns), as well as by ultraviolet and other types of radiation (radiation burns). In peacetime, the main place is occupied by thermal burns as a result of carelessness in everyday life (scalding with boiling water), fires, rarely due to industrial injuries due to non-compliance with safety measures. The most common radiation burns are sunburn. Burns as a combat injury can be caused by the use of incendiary mixtures, as well as nuclear weapons, the light radiation of which causes skin burns and damage to the organs of vision.
The most common are flame burns, which were detected in 84.3% of more than 1000 patients who were in the hospital. The second place was taken by liquid burns (7.2%), the third - electric burns and burns by an electric arc flame (6.4%). Burns caused by other factors were observed in 2.1% of patients.
In modern conditions of intensive industrialization, the ever-increasing use of heat sources in production and in everyday life, there is a tendency to an increase in the frequency of burns. According to the World Health Organization, burns rank third among other types of injuries, and in Japan - second, second only to transport injuries, in peacetime burns account for 5-12% of all types of injuries. Analysis of literature data suggests that burns occur everywhere in 1 person per 1000 population. The incidence of burns can depend on a number of conditions: the level of development of the national economy, the nature of production, transport, living conditions, etc. It rises sharply in conditions of war, the use of nuclear weapons and incendiary mixtures. Burns are often fatal, and among those who have recovered, many remain disabled.
2.Classification of thermal damage
2.1 Thermal skin burns
Coagulation of skin proteins occurs from exposure to high temperatures. Skin cells die and undergo necrosis. The higher the temperature of the traumatic agent and the longer its exposure, the deeper the damage to the skin. There are four degrees of burns: I degree - persistent hyperemia, II degree - exfoliation of the epidermis and blistering. III degree - burnout of the skin itself (dermis). Burns of the III degree are divided into superficial - III a degree and deep - III b degree; IV degree - burnout of the skin, subcutaneous tissue and deeper structures.
2.2 Frostbite
Local exposure to low temperatures causes a pathological process in the tissues - frostbite. The latter can also occur at a positive ambient temperature in conditions of other unfavorable factors - high humidity, wet clothes, strong winds, tight wet shoes, starvation, blood loss.
There are four degrees of frostbite: Superficial frostbite (I - II degree) heal on its own - epithelialization without scarring. With frostbite II degree, the growth layer of the skin is preserved. Blisters on the skin with transparent contents are characteristic. Epithelialization occurs in 1.5-2 weeks. The degree of frostbite is characterized by necrosis of the skin throughout its depth. After scab rejection, healing is possible only with the formation of scars. Grade IV frostbite is characterized by necrosis not only of the skin, but also of deep tissues, including bones. The formation of thick-walled blisters with dark hemorrhagic contents is possible. Demarcation and rejection of necrosis occurs for a very long time, amputation is often indicated.
2.3 General cooling (freezing)
light (adynamic) - with a decrease in body temperature to 34-32 degrees;
moderate (stuporous) - at a body temperature of 31-29 degrees;
severe (comatose) - at a body temperature of 28-26 degrees.
A drop in body temperature below 25-23 degrees leads to the clinical death of the victim.
2.4 Clinical signs of thermal injury
Burns of I-II degree are superficial and heal without scarring. Third degree burns are deep, accompanied by scarring. For their healing, it is often necessary to resort to free skin plastic surgery. With IV degree burns, necrosis of the limb may occur, requiring amputation.
Burns of the first degree are characterized by persistent hyperemia of the burned skin, severe pain; with burns of the II degree against the background of hyperemic skin, bubbles of various sizes are distinguished, filling with transparent contents; with third-degree burns against the background of areas of hyperemia, open blisters, areas of white ("pig") skin with scraps of epidermis are visible; IV degree burn - skin charring. Extensive burns (superficial - more than 30% of the skin area, deep - more than 10%) are complicated by Burn Shock, characterized by a prolonged erectile phase with psychomotor agitation, moderately elevated blood pressure. The victims rush about in pain, strive to escape, they are poorly oriented in the place and situation. Excitation is replaced by prostration with a fall in blood pressure. Burn shock is characterized by blood thickening due to large plasma loss. There is little urine, it is sharply concentrated, and in severe burns of a dark color due to the admixture of hemolyzed blood.
2.5 Frostbite
Unlike burns, in case of frostbite, exposure to low temperatures does not directly lead to tissue necrosis. It occurs a second time, in the reactive period, due to vasospasm, blood stasis in them and thrombus formation with subsequent changes in the vascular wall itself. The endothelium swells and infiltrates, followed by connective tissue degeneration and the development of vascular obliteration.
During frostbite, 2 periods are distinguished: latent (pre-reactive), in which the affected areas are pale, devoid of sensitivity, but it is impossible to determine the depth and area of \u200b\u200bfrostbite during this period. The latent period lasts for several hours (up to a day). After warming the limb and restoring blood circulation in it, the second period begins - reactive. In the first 12 hours from the beginning of rewarming, the early reactive period is characterized by microcirculation disorders and thrombus formation. The subsequent late reactive period is characterized by the development of subsequent tissue necrosis, infectious complications, increasing intoxication, anemia.
In the reactive period, it becomes possible to determine the depth of the lesion. Distinguish frostbite of 4 degrees.
Superficial frostbite (I - II degree) heal on its own - epithelialization without scarring. With frostbite II degree, the growth layer of the skin is preserved. Blisters on the skin with transparent contents are characteristic. Epithelialization occurs in 1.5-2 weeks. The degree of frostbite is characterized by skin necrosis throughout its entire depth. After scab rejection, healing is possible only with the formation of scars. Grade IV frostbite is characterized by necrosis not only of the skin, but also of deep tissues, including bones. The formation of thick-walled blisters with dark hemorrhagic contents is possible. Demarcation and rejection of necrosis occurs for a very long time, amputation is often indicated.
Long-term repetitive cooling of the legs in a humid environment, even at above-zero temperatures, leads to the development of a kind of cold injury, which is called "trench foot". The defeat is manifested by aching pains in the feet, a feeling of "woodiness", burning. Feet are cold, swollen. Blisters with hemorrhagic contents appear. The body temperature rises, weakness, tachycardia increase, infectious complications join.
2.6 Freezing
The adynamic stage of general cooling is characterized by increasing weakness, drowsiness, chanting speech, decreased heart rate (60 per 1 minute), thirst, and chills. The skin takes on a marbled appearance - an alternation of pale areas (spots) with cyanotic ones. In the stuporous stage, further suppression of functions occurs: consciousness is depressed, movements are difficult, limited, breathing is rare (10 in 1 minute), bradycardia increases (up to 40 in 1 minute), the pulse is weak, the skin is cold, bluish-pale. Blood pressure decreases. In the comatose stage, consciousness is absent, the reaction of the pupils to light is sharply reduced. There are tonic convulsions of the limbs with rigor (stiffness). Breathing is shallow, rare (5 in 1 minute), the pulse is reduced by about 30 in 1 minute, blood pressure is sharply reduced. In a state of clinical death, the pulse, blood pressure, heart sounds are not detected, breathing is absent, areflexia is noted, and the corneal reflex is absent.
2.7 Eye burns
Accurate diagnosis of the severity of eye damage with burns is very difficult, since in the first hours and days after the injury it may look light, and after 2-5 days, severe irreversible changes in tissues, especially the cornea, may appear, up to its perforation and eye death. In this regard, all patients with eye burns after providing emergency first aid or non-specialized medical care at the site of the lesion should be urgently delivered to the nearest trauma center operating around the clock on the basis of the inpatient ophthalmological department.
Photophobia, eye pain, eyelid spasm, redness, swelling of the eyelid and conjunctival skin, decreased vision with all degrees of burn. Burns of the 1st degree (light) are characterized by superficial lesions of the epithelium of the eye tissues in the form of redness and slight edema of the skin of the eyelids and conjunctiva, slight edema of the corneal epithelium, less often epithelial erosion.
Second-degree burns (moderate) are characterized by damage not only to the epithelium, but also to the surface layers of the eyelid skin itself, subconjunctival tissue and corneal stroma, which is manifested by the formation of blisters on the skin, superficial films and erosions on the conjunctiva and cornea. Burns of the third degree (severe) occur with damage and necrosis of the deeper layers of the eye tissues and occupy half or less of the surface of the eyelid, conjunctiva, sclera and cornea in area. Tissue necrosis looks like a white, gray or yellow scab, the conjunctiva is pale, ischemic, edematous, episclera is affected, the cornea looks like frosted glass. Burns of the IV degree (especially severe) are characterized by even deeper necrosis of the eye tissues, occupying the entire thickness of the skin, conjunctiva, muscles, eyelid cartilage, sclera and cornea, and in terms of the affected area - more than half of the tissue surface. The scab of necrosis looks gray-yellow or brown, the cornea has a white porcelain appearance.
Agents in peacetime: hot steam, water, oils, flames, molten metal, chemical mixtures (contact burns). Burns by steam, liquids are more often combined with damage to the skin of the face, body, limbs, however, the eyeball itself is affected less often and less severely due to the reflex of the quick closing of the palpebral fissure and at a low temperature of the damaging agent (up to 1000 ° C). Contact burns differ in considerable depth with a small area of \u200b\u200bthe lesion. In wartime, with the use of combustible mixtures and thermonuclear weapons, the proportion of thermal burns increases. For example, napalm, the ignition of which gives a temperature of 600-800 ° C, causes extensive severe burns, more often III and IV degrees. Thermal and thermochemical eye burns, as a rule, occur against the background of general burn disease as a result of burns of the face and other parts of the body.
2.8 Burn disease
Limited superficial burns are usually relatively easy and heal within 1 to 3 weeks without affecting the general condition of the victim. Deep burns are more difficult. Damage to tissues on an area of \u200b\u200bup to 10%, and in young children and seniors up to 5% of the body surface is accompanied by severe disorders of the activity of all body systems as a result of strong thermal exposure. An intense flow of nerve-pain impulses from a large area of \u200b\u200bthe burn leads to a disruption in the relationship between excitation and inhibition processes, and then to overstrain, exhaustion and a sharp disruption of the regulatory function of the central nervous system.
Disturbances in the central and peripheral nervous system arising under the influence of burn injury lead to pathological reactions and morphological changes in the cardiovascular, respiratory, endocrine, immune systems, blood, kidneys, liver, and ventricular tract. The victims develop disorders of all types of metabolism and redox processes, burn disease develops with a variety of clinical manifestations, which are based on neurodystrophic processes.
In the pathogenesis of burn disease, disorders of systemic hemodynamics and microcirculation, pronounced metabolic changes, characterized by a catabolic orientation and increased proteolysis, are of great importance. During a burn disease, it is customary to distinguish between periods of shock, acute toxemia, septicotoxemia and recovery, or convalescence.
Burn shock is the body's response to a super-strong pain stimulus. It is based on thermal trauma, leading to severe disorders of central, regional and peripheral hemodynamics with a predominant violation of microcirculation and metabolic processes in the body of the burned person; there is a centralization of blood circulation.
Prolonged painful irritation leads to dysfunction of the central nervous system, endocrine glands and the activity of all body systems.
Hemodynamic disorders are characterized by hemoconcentration, a decrease in MOS and BCC due to plasma loss, and insufficient blood supply to tissues. The victims develop tissue hypoxia and acidosis, diuresis decreases, there are pronounced violations of the water-electrolyte balance, protein, carbohydrate, fat and other types of metabolism, the basal metabolism increases sharply, progressive hypo and dysproteinemia develop, deficiency of vitamins C, group B, nicotinic acid. The development of hypoproteinemia is facilitated by the increased breakdown of tissue proteins, their loss through the wound due to an increase in the permeability of the capillary walls. The volume of circulating erythrocytes decreases due to their destruction in damaged tissues at the time of injury, and to a greater extent - as a result of pathological deposition in the capillary network due to microcirculation disorders.
Despite hemodynamic disorders, blood pressure in the first hours after injury can remain relatively high, which is explained by an increase in the total peripheral resistance to blood flow, which occurs due to vasospasm caused by an increase in the activity of the sympathoadrenal system, as well as an increase in blood viscosity due to hemoconcentration and deterioration of its rheological properties.
Burn shock is observed with burns, the area of \u200b\u200bwhich is not less than 10-15% of the body surface. In children and people over 60 years of age, manifestations of burn shock can be observed with a smaller lesion area.
According to the severity and duration of the course, light, severe and extremely severe burn shock are distinguished.
The duration of the burn shock is 24-72 hours. The criteria for recovering from the state of shock and transition to the second period of the burn disease are stabilization of hemodynamic parameters, restoration of BCC, IOC, absence of hemoconcentration, reduction of tachycardia, normalization of blood pressure and urine output, increase in body temperature.
Diagnosis of shock is based on determining the total area of \u200b\u200bburns and the so-called Frank index (IF), identifying hemodynamic disturbances and renal excretory function. The total area of \u200b\u200bthe burn includes superficial and deep lesions. IF - the total value of superficial and deep burns, expressed in units. The Frank index suggests that a deep burn affects a person 3 times more than a superficial one. In this regard, 1% of superficial burn is 1 unit. IF, and 1% deep - 3 units. IF. Concomitant respiratory tract damage is equivalent to 15-30 units. IF.
3. Methods of treatment and rehabilitation for thermal injuries
medical thermal injury paramedic
Outpatient treatment is possible with extensive burns of I degree, burns of II and IIa degree not more than 5% of the body surface, mainly functionally inactive areas.
The victims with limited deep thermal and chemical burns are operated on and treated in a trauma center. It is possible to perform necrosectomy and free skin grafting only in a surgical hospital, where the operated person must stay at least until the first dressing, that is, at least 5-7 days.
Patients discharged from hospitals must also complete treatment in polyclinic medical institutions. The main task of the outpatient treatment of such patients is the earliest possible restoration of their ability to work, that is, rehabilitation.
First aid to a burned person who applies to a polyclinic medical institution immediately or early after an injury should be provided in compliance with the basic rules set forth earlier. Limited first-degree burns, even in outpatient settings, have to be observed extremely rarely only because such victims almost always self-medicate (cooling the burn areas with water, treatment with alcohol, cologne, etc.) and do not seek medical help.
In such cases, it is advisable to use a cooling cream (lanolin, peach oil, distilled water in equal parts), slightly disinfecting (2% boric petroleum jelly) ointments containing corticosteroid hormones (prednisolone ointment, oxycort), indifferent shaken mixtures (zinc oxide, talcum powder, 30 g, distilled water 100 ml). There is no need to apply a bandage. Hyperemia and edema are eliminated within 3 - 5 days, pains disappear much earlier.
If the victim handles a bandage already applied at the scene of the incident, after its removal, the area and depth of the lesion are determined. After making sure that the patient can be treated on an outpatient basis, you should immediately make a primary toilet for II-III degree burns. Since this manipulation, if it is performed skillfully and carefully, with limited burns is not traumatic, the preliminary administration of narcotic analgesics is not required.
The skin in the circumference of the burn, as well as its surface, if the integrity of the exfoliated epidermis is not violated, is cleaned with alcohol or washed with a 0.25% solution of ammonia. Large bubbles are cut, the exfoliated epidermis is cut off. Small bubbles can be left unopened. Excessively careful removal of the epidermis, increasing the duration and trauma of the primary burn toilet, does not significantly affect the subsequent healing of burn wounds.
After the toilet, the surface of the burn is closed with an emulsion-ointment dressing (Vishnevsky ointment, 5 and 10% synthomycin emulsion, 0.5% furacilin ointment and other similar agents). If these ointments are not available, antiseptic solutions or other treatments for burns can be used. It is perfectly acceptable to limit yourself to the imposition of a dry aseptic dressing. Anti-tetanus serum with toxoid is introduced.
In case of second-degree burns, the first dressing on the 7-8th day after the injury, in principle, may be the last. By this time, epithelialization of the burned surface occurs and the bandage is no longer needed. If there are unhealed areas of a third-degree burn, dressings are made in 1-2 days until their complete epithelialization.
An indication for earlier removal of the bandage is a suspicion of the development of acute purulent inflammation, manifested by increased pain in the burn wound, sometimes acquiring a pulsating character, blotting the bandage with pus, regional lymphadenitis, edema in the circumference of the burn, sometimes a significant increase in body temperature, chills.
Examination of the burn wound, assessment of the state of regional lymph nodes and other symptoms allow us to establish the nature of the complication.
With burns of the II degree, suppuration of the wound surface and fluid of unopened burn blisters does not affect the timing and outcomes of healing. At the same time, in case of burns with necrosis of the dermis (partially or to the full depth), demarcation and rejection of dead tissues are necessarily accompanied by the development at the end of the first - beginning of the second week in varying degrees of pronounced purulent-demarcation inflammation. In such cases, it is an indispensable component of the wound process. Therefore, with suppuration of a burn wound, the depth of the lesion should be carefully evaluated again and, if areas of deep burn are identified, the patient should be hospitalized.
If you decide to continue treatment on an outpatient basis, you should repeat the toilet of the burn wound, completely removing the exfoliated epidermis and pus-filled blisters that have not been opened earlier. The wound surface is thoroughly washed with a solution of hydrogen peroxide or an antiseptic, after which a bandage is applied with an antiseptic solution. With a deterioration in health, chills, high fever, it is advisable to prescribe broad-spectrum antibiotics. Antibiotic therapy should be corrected depending on the clinical effectiveness of its use and laboratory data on the sensitivity of the microflora of burn brine to antibiotics. The same should be the tactics for the occasionally observed erysipelas, lymphadenitis and lymphangitis. As a rule, acute inflammation in superficial burns quickly subside and does not significantly increase the duration of treatment.
Studies carried out in the clinic for thermal injuries have shown that 3.3% of patients with limited superficial burns develop various dermatoses in the early stages after injury. Of these, the most common are peri-wound pyoderma.
They flow for a long time, and after healing of burns they often recur. It should be borne in mind the possibility of dermatitis arising from intolerance to the medications used (antibiotics, sulfa drugs, amprovizole, fastin), or the irritating effect of disinfectants. Sometimes dermatitis develops from the use of ointments made on the basis of petroleum jelly. One of the causes of dermatitis may be a rare change of dressings on festering burn wounds. To combat pyoderma, careful disinfection of the skin surrounding the burn is necessary, the use of aqueous or alcoholic solutions of aniline paints, 1% hex-chlorafenic or 5% boron-naphthalene ointments on the affected areas. In case of allergic dermatitis, the medication used should be changed.
In case of burns of functionally active areas, 3 days after the injury, it is necessary to start physical therapy in order to accelerate the recovery of function. Initially, active movements are used with minimal muscle load and limited amplitude, which do not cause pain. Movements in the joints of the affected area should be combined with exercises for a symmetrical unaffected limb. A prerequisite for the effectiveness of physical therapy classes is their regularity and a gradual increase in the load.
It is especially important to use this method for burns of the hands. Slow painless movements in the joints of the hand and fingers at the maximum possible amplitude (flexion, extension, opposition) should be supplemented with exercises to strengthen the muscles (squeezing a soft sponge in a bath after soaking the dressing). The most important exercises are those that restore grip functions and coordination of movements. For this, folding of matches, cubes, mosaics, weaving of braids from a ribbon, possibly an earlier restoration of household skills are used.
In case of II degree burns, these measures allow restoring the function of the hand in 1.5-2 weeks, and in case of III degree burns 4-6 weeks after injury.
In case of burns of the legs and feet, considerable attention should be paid to restoring the support ability of the lower extremities. Pain in the areas of burns, aggravated by standing up, forces the victims to lie down for at least 6-7 days after the injury. Even after the epithelialization of the burns, several days pass before the burned person becomes able to walk in ordinary shoes. Full recovery of the limb support ability occurs at the end of the third - at the beginning of the fourth week with burns of the II degree, and with burns of the IIIa degree, this period increases by 1.5 - 2 times.
To speed up the restoration of the support ability of the lower extremities, physical exercises are necessary from the first days after the injury - frequent changes in the position of the limbs, dorsal and plantar flexion in the ankle joint, abduction, adduction and circular movements of the foot. After the start of walking, you need to monitor the correctness of the movements - to achieve the natural extension of the leg, the placement of the foot, its roll. If these requirements are not followed, gait may turn out to be pathological even after the complete restoration of joint mobility.
A special, still very little studied and very important problem is the rehabilitation of burned, discharged from the hospital. Usually, outpatient treatment of such patients is reduced mainly to conservative treatment by bandaging small wounds left after superficial burns and around the engrafted grafts in those operated on for deep burns. This is not enough in patients who have undergone severe burn disease, as well as with various post-burn deformities, late dermatoses.
4. Features of rehabilitation after discharge from the hospital
It is advisable to distinguish the following groups of pathological conditions:
) dysfunction and cosmetic defects after conservative treatment of superficial, including extensive burns;
) dysfunction and cosmetic defects remaining after surgical treatment of IIb degree burns;
) the consequences of IV degree burns, as well as mutilation interventions: amputations, exarticulations, resections of the joints, performed for the death of a limb segment due to a deep burn;
) late dermatoses;
) various functional disorders and diseases of internal organs, which are the result of burn disease or its complications.
Rehabilitation of survivors of superficial burns is mainly reduced to physical therapy, as applied to the outpatient treatment of limited superficial burns. It is necessary to bear in mind the possibility of developing keloid scars after III degree burns, especially in patients predisposed to their formation. If such scars are a significant cosmetic defect, treatment with pyrogenal or the introduction of lidase with corticosteroid hormones into the scar tissue should be performed. Sometimes satisfactory results are achieved after using electrophoresis with ronidase, ultrasound with hydrocortisone emulsion, 70% dimethyl sulfoxide solution. If conservative treatment is unsuccessful, there is a need for surgical correction of scars, which should be undertaken in a specialized department for the treatment of burns and their consequences.
The same methods should be used in the rehabilitation of patients who underwent surgical restoration of the skin in the areas of burns of the IIIb degree. The main task is to stretch the scars, accelerate their maturation, as well as prevent irreversible graft reactions.
This is achieved mainly by passive movements in the joints, performed with the help of an exercise therapy methodologist. To combat contractures, it is important to strengthen antagonist muscles, which is achieved by active strength exercises and relaxation of muscles in a state of contraction, for which small amplitude movements with unloading are carried out. The set of exercises used is determined by the exercise therapy methodologist, depending on the period that has passed since the moment of injury, developed local changes and localization of the burn.
The effectiveness of physical therapy increases if it is used with massage and physiotherapy procedures. In the early stages after epithelialization of wounds, warm (35-40 ° C) baths, sollux should be used. As the scars form and the strength of the epithelium covering them increases, paraffin applications should be made before physical therapy. The massage should be done carefully so as not to injure the young epidermis. This procedure significantly accelerates the normalization of blood circulation and lymph circulation, contributes not only to deretraction of scars and operatively restored skin, but also to an increase in the elasticity of deeper anatomical structures that are also involved in the development of contracture. In addition, the massage stretches the surrounding intact skin, which increases the range of motion. Sometimes the range of motion achieved during exercise therapy decreases after a few hours. To prevent this undesirable phenomenon, it is advisable to immobilize the joint in the position that was achieved at the end of the session.
It is especially important not to waste time for the production of those interventions, the delay with which threatens the development of severe consequences (keratitis with ulceration of the cornea and loss of vision with cicatricial eversion of the eyelids, impaired bone growth due to cicatricial deformities in children). Such patients should be promptly referred to restorative surgery facilities.
The most difficult rehabilitation after burns of the IV degree, leading to severe dysfunctions due to the destruction of deep anatomical structures (tendons, joints, bones) or disfigurement with the loss of part or all of the organ (nose, ears, fingers and toes). These patients should be referred to surgical hospitals for reconstructive or maxillofacial surgery. The question of rehabilitation of those who have suffered deep burns of the cranial vault, especially in the presence of bone defects, should be resolved with the participation of a neuropathologist and neurosurgeon. In case of ankylosis and deforming arthrosis that have developed after postponed purulent arthritis, it is necessary to consult an orthopedic traumatologist to assess the indications for reconstructive interventions (arthroplasty, tendoplasty, arthrodesis in a functionally advantageous position). To partially restore the function of the hand after the loss of fingers, especially fingers I, in a number of patients, it is advisable to apply phalangization of the first metacarpal bone, transplantation of any of the remaining fingers on the vascular pedicle to the place of the first finger, or its formation with the Filatov stem.
For those who have undergone amputations of large segments of the limbs, the leading link in rehabilitation is prosthetics. It can be carried out on an outpatient basis only after typical amputations, mainly of one of the upper limbs. After multiple amputations, as well as in cases where the limb was truncated distal to the level of a deep skin burn, and the skin on the stump was restored promptly, prosthetics are usually difficult. It is especially complicated by the diseases and defects of the stumps that often develop in such cases. Their elimination requires long-term treatment in a specialized hospital, where prosthetics and training in the use of a prosthesis should also be carried out.
Thermal injury classification is based on indicators such as the area and depth of the affected tissue.
Clinical manifestations depend on the damaging factor and the volume of destroyed tissues.
Rehabilitation methods for thermal injuries are aimed at restoring the physical, mental, professional, social and economic value of such patients.
5. Investigation of the features of paramedic activity during various rehabilitation methods in order to improve the quality of life of patients with thermal injuries
Table 1. Generalized statistical indicators.
Country Russia Total burns 0.5 million people are treated on an outpatient basis 390-400 thousand 80% Hospitalized 100-110 thousand 20%
5.1 Quantitative analysis of patients with thermal injuries at the FAP site
The research work was carried out on the basis of BUZ VO "Rossoshanskaya RB". To determine the role of the paramedic in the provision of first aid for thermal injuries, treatment and prevention, it was decided to analyze the records in the outpatient cards of the FAP of a rural settlement for 2015, in which cases of treatment of persons living in the territory of this settlement with regard to thermal injuries, as well as described the actions of a paramedic during rehabilitation measures.
As a result of the study, the following data were obtained:
the total number of complaints in connection with thermal injuries was 72 people.
table 2
Degree of burn Number of calls Cause I38 Hot water, steam II20 Flame III8 Flame IIIa6 Flame IV0 Flame TOTAL 72
The result of the analysis of records in outpatient cards by age criteria.
The percentage is as follows:
Age 18-30 25%;
45 years 37%;
60 years old 23%;
years and over 15%.
5.2 Methods of rehabilitation of patients with the participation of a paramedic in a FAP
Tactics at the prehospital stage: - cessation of the effect of the damaging factor; - removal of the victim from the thermal action zone; - the imposition of a protective aseptic bandage; - the introduction of anesthetics, drugs to prevent shock; - the use of transport immobilization for extensive and deep burns; - the introduction of cardiovascular funds and antibiotics according to indications; emergency hospitalization in the surgical department of the hospital.
In accordance with the content of records in the outpatient cards of the FAP:
38 patients (I degree), the area of \u200b\u200bthermal damage was treated with a 33% alcohol solution, recommendations were given for the care and toilet of damaged surfaces;
20 patients (II degree), the area of \u200b\u200bthermal injury (5 foot surface, 15 hand) was treated with 33% alcohol solution, a sterile dressing with 0.2% furacilin ointment was applied, recommendations were given for the care and toilet of damaged surfaces;
In 14 patients (III degree), the area of \u200b\u200bthermal injury was treated with a 33% alcohol solution, before hospitalization, bandages with 0.2% furacilin ointment, 5% streptocidal ointment were applied to the burn surfaces; by the paramedic and FAP staff, hospitalization was organized in the surgical department of the Central District Hospital.
Feldsher activity in the rehabilitation of patients with the consequences of thermal injuries of the II, III and IIIa degrees.
It is advisable to divide the rehabilitation of post-burn convalescents into 3 stages. The first stage is early, starting immediately after the patient is discharged from the hospital with healed burn wounds, when conservative rehabilitation is required. The second stage is surgical rehabilitation. And the third stage is the final one, when conservative follow-up care, expansion and stabilization of the restored functions are carried out.
At the beginning of the first stage of the post-burn rehabilitation period, four groups of post-burn reconstructions are distinguished:
) who do not need special follow-up treatment;
) in need of physiotherapy and restorative treatment;
) subject to relatively urgent surgical interventions;
) requiring a systematic complex conservative treatment.
Physiotherapy and restorative treatment for patients of group 2 is carried out outside working hours with the appropriate equipment.
Reconvalescents of 3 groups requiring relatively urgent operations (sharp contractures of the joints, neck, perineum, eversion of the eyelids) are sent to rehabilitation centers, burn centers or burn departments of regional hospitals.
The fourth group of convalescents, who are under dispensary supervision and need complex conservative treatment at the 1st stage of rehabilitation, is the main one both in terms of the volume of therapeutic measures carried out and the consequences, which will largely be determined by the thoroughness of the implementation of the rehabilitation program.
Patients with the sequelae of grade II, III and IIIa thermal injuries presented identical complaints of pain and muscle tension.
During the examination, motor and sensory disorders were determined.
For anesthesia, dynamic currents were applied to the area of \u200b\u200bhyperalgesia in a push-pull current mode (for 2 min) and a current modulated with long periods. The electrode, connected to the cathode, was located in the zone of hyperalgesia at the nerve exit point. The analgesic effect was manifested during the procedure. The effectiveness of anesthesia increased when the pads were wetted with a solution of 2% lidocaine solution. With the open method of treatment, local electric light baths were used for 2-3 hours / day. Aeronization was carried out with negatively contaminated ions. For burns of fingers, feet, or joints, a paraffin-oil bandage (1 / part of fortified fish oil and 3 / part of paraffin) was used.
For thermal burns in the acute period, segmental reflex massage was used to eliminate the pain factor and inflammatory edema. For this purpose, the intercostal spaces, sternum, costal arches and ridges of the iliac bones were rubbed. Compression, stretching and concussion of the chest was applied. When the burn was localized on the lower extremities, the paravertebral zones of the lumbar and lower thoracic spinal segments were massaged.
Massage of the burn surface is started at the stage of scarring. After exposure to thermal paraffin-oil applications, the following were used: stroking, rubbing with fingertips, shading, sawing, spanking, longitudinal and transverse kneading, stretching, shifting, with persistent contractures - redressing movements. The duration of the procedure was 5-20 minutes daily or every other day.
Exercise therapy technique for burns
Exercise therapy is indicated for all patients, regardless of the degree of the burn, its localization and the area of \u200b\u200bthe lesion. Contraindications for exercise therapy are:
burn shock; severe general condition;
severe complications: hepatitis, myocardial infarction, nephritis, pulmonary edema; - risk of bleeding (if burns are localized in the area of \u200b\u200bthe great vessels);
suspicion of latent bleeding.
Exercise therapy tasks:
) normalization of the activity of the central nervous system, CVS and the respiratory system;
) prevention of complications (pneumonia, thrombosis, intestinal atony);
) improvement of trophic processes in damaged tissues;
) preservation of mobility in the joints of damaged body segments;
) prevention of dysfunction in unaffected limbs (prevention of contractures, muscle atrophy, tightening scars).
To solve the above tasks, the following complex was used.
Physical therapy consisted of 3 stages: introductory, main and final. At the introductory stage, general tonic and breathing exercises were carried out with a small load; on the main - special exercises corresponding to the location and nature of the lesion. At the final stage, the load gradually decreased, the pace of the exercises slowed down with an emphasis on breathing movements. The duration of each stage depended on the patient's condition and the program planned for him. Physiotherapy exercises in some patients were individual, group and independent, under the direct supervision of a specialist or on his recommendations.
I. p. - sitting on a chair; legs slightly apart, palms on knees, back straight. Raise straight arms forward, upward - inhale (look at the hands). Return to and. n. - exhale. Repeat 5-0 times.
I. p. - sitting on a chair; hands on the belt - inhale, tilt to the side - exhale. Repeat 4-5 times in each direction.
I. p. - the same; raise your arms to the sides - inhale. Raise the bent leg slightly, placing both palms on the knee - exhale. Repeat 4-6 times with each leg. To increase the load, hug the knee with your hands and, while exhaling, raise it higher.
I. p. - sitting on a chair; turning the body to the left; take your straight left hand back to the side, look at the palm, return to and. n. exhale. Repeat 3-5 times in each direction.
I. p. - the same; lower your arms and take your shoulders back, bending in the chest - inhale. Having made a slight bend forward, put your hands (fingers inward) on your knees - exhale. Repeat 5-0 times. To increase the load, spread your legs wider and make a tilt alternately to each knee - exhale, putting your palms on the knee and spreading your elbows wider.
I. p. - the same; get up, raise your hands up - to the sides - inhale, return to and. p. - exhale. Repeat 4-6 times. To increase the load, the exercise is performed with dumbbells.
I. p. - standing behind the back of the chair; feet together, palms resting on the back of the chair. Raise a straight leg to the side - inhale, lower it into and. p. - exhale. Repeat 4-5 times with each shoulder strap.
Rise on your toes - inhale. Roll down onto your heels - exhale (lift your socks up). Repeat 6-10 times.
I. p. - standing, holding the back of the chair; sit down - exhale, return to and. p. - inhale. To increase the load, do 2 spring squats.
I. p. - the same, when turning the body to the right; take the right straight hand back as far as possible (clench the hand into a fist) - inhale, return to and. n. - exhale. Repeat 5-6 times in each direction. To increase the load, take your hands away with springy jerks (2-3 jerks in a row).
I. p. - raise one hand up, put the opposite leg back on the toe - inhale, return to and. n. - exhale. Repeat 3-5 times with each leg and arm.
Walk for 1 - 2 minutes, breathing deeply (2 - 3 steps - inhale, 4 - 8 steps - exhale). Walking can be replaced by walking on the spot.
I. p. - sitting on a chair, arms forward. Squeeze and unclench your fingers, breathing is free. Repeat 10-15 times. Clench your fingers into fists and make 5-10 circles in the wrist joints alternately in both directions, then shake loosely with your hands.
Repeat exercise. 1 5 - 6 times.
6. Medical assessment of the effectiveness of rehabilitation measures
with the participation of a paramedic in patients with thermal injuries
In the process of physiotherapy and massage, complaints about pain, general weakness, and fatigue decreased. Sleep improved. Physiotherapy was carried out regardless of the degree of the burn, its localization and the area of \u200b\u200bthe lesion. Physical exercises increased the general tone of the autonomic nervous system, ensured an increase in the speed of blood flow, improved microcirculation, positively influenced the function of respiration, increased emotional mood, gave confidence in their abilities,
The rehabilitation measures carried out were an effective method of restorative treatment of patients with thermal injuries, improving their quality of life.
Conclusion
As applied to patients with thermal injuries, it seems appropriate to define rehabilitation as a system of measures carried out after complete or almost complete healing of burn wounds resulting from conservative or surgical treatment and elimination of acute manifestations of burn disease. For some patients, rehabilitation can be carried out from beginning to end in general polyclinics. In a number of patients who have suffered burns, there is a need for repeated hospitalizations to deal with the consequences, the correct assessment of which and the timely referral of victims to a specialized medical institution, after consultations, if necessary, with the appropriate specialists, is an important task of the polyclinic staff.
The rehabilitation technique, its duration and expected results are determined by a number of factors, the main of which are: the area of \u200b\u200bburns, especially deep ones, their localization, the presence or absence of primary or secondary lesions of deep anatomical structures, the method of treatment of burns, their complications, and the peculiarities of the course of burn disease. Naturally, this determines the variety of necessary rehabilitation measures, in which the paramedic is assigned a significant role.
The purpose of this course work was to analyze the role of a paramedic in carrying out rehabilitation measures for patients with thermal injuries to improve their quality of life.
To achieve the goal set in the course work, the following tasks were solved:
The anatomy of tissues exposed to thermal factors is considered.
The most common causes of thermal damage are noted.
Thermal damage classified.
Methods of treatment and rehabilitation for thermal injuries are described.
The paramedic activity in carrying out rehabilitation measures has been determined.
The effectiveness of the performed rehabilitation has been analyzed.
The object of the study was thermal damage.
The subject of analysis is the role of a paramedic in carrying out rehabilitation measures for patients with thermal injuries in order to improve the quality of life.
During the course work, the literature on anatomy, combustiology, methods of rehabilitation for thermal injuries, and organization of paramedic activities were used.
For the implementation of the practical part, the data from the records in the outpatient cards of the FAP of a rural settlement were used.
The coursework consists of two chapters. The first chapter discusses
anatomy, clinical manifestations, methods of treatment and rehabilitation for thermal injuries.
The second chapter, which is a practical part, provides a statistical analysis of the cases of patients' appeals to the FAP paramedic associated with thermal injuries, as well as paramedic activities during rehabilitation measures.
Based on the results of the work carried out, it seems possible to draw the following conclusions:
Today, the problem of thermal injuries retains its importance in practical surgery.
Physiotherapy, massage and exercise therapy are used for physical rehabilitation of patients with thermal injuries. These techniques allow in a relatively short time to restore the functionality of patients and, as a consequence, improve their quality of life.
The direct participation of a paramedic in rehabilitation activities increases their overall effectiveness.
Bibliography
1. Ariev T.Ya. Burns and frostbite. L., "Medicine", 1966.
Ariev T. Ya. Thermal lesions. L., "Medicine" 1971.
Ataev Z.M. , Vinogradova O.I. , Korolev L.F., Sagirov E.A., Elagina V.
A. Technique of functional treatment of patients with burns - "Tr. Moscow. Scientific - issled. Institute of Emergency Medicine. Sklifosovsky Research Institute for Emergency Medicine, 1971, issue. 17.
Bogolyubov V.M. Patient therapy doctor, today, tomorrow. Physiotherapy, sickness, rehabilitation. - 2002, No. 1.
Butyrina G.Ya. “Physiotherapy for burns. L., "Medicine", 1965.
Medical Rehabilitation Guide. Edited by V.M. Bogolyubov in 3 volumes / M., 1998, - 599s
V. I. Dubrovsky Massotherapy. - M., 2001. Nikolova and prof. St. Boynikeva Special physiotherapy. Medicine and physical education Sofia - 1974
Sokrut V.P. Medical rehabilitation in the clinic of internal diseases. - Donetsk, 2001.
Popova S.N. Physical rehabilitation edition 2 - Rostov N / A: publishing house "Phoenix", 2004.
Physiotherapy exercises Edited by V.A. Epifanov. - M., "Medicine", 1987.
A guide to the rehabilitation of the burned. V.V. Yudenich V.M. Grishkevich - medicine 1986
Sitkovsky N.B. Dolnitskiy O.V. Treatment of post-burn deformities of the perineum. 1978.
Bulletin of surgery. Named after I.I. Grekov. Leningrad "Medicine"
Ushakov A.A. - Pain relief by physiotherapy. - Moscow, Military Medical Journal 1992.
Questions of balneology, physiotherapy and physical therapy.
Lvova N.V. , Komarova L.A. Application of ultraviolet radiation
in physiotherapy and cosmetology. - Moscow. , 2007
Karpukhin I.E. The main directions and prospects for the development of medical rehabilitation. Moscow. , 2007 Scientific - practical journal.
Klyachkin Ya.M., Vinogradova M.N. Physiotherapy: Textbook. 2nd ed. , The medicine. 1995
Sytnik A. A., Beletskiy A. V. Comparative characteristics of treatment methods for burns №4.
Yurina T. M. O. A. Rozhenetskaya. Moscow. , 2007 Scientific - practical journal. Burns.
Physiotherapy and therapeutic - physical culture Gelfond V. B. - Moscow. , 2007
Mikhailovsky M.V., Khanaev A.L., Gubina E.V. Effect of ultraviolet irradiation 1995. The medicine.
Babko A.M., Gerasimenko S.I., Ivanchenko L.A. Artificial general UFO. Scientific - practical journal. Doctor. 2007
Chapter 1 The main structure of the work of a paramedic at FAP
Organization of work at the feldsher-obstetric station (FAP)
Description of the feldsher-obstetric station
The feldsher-obstetric center is an outpatient clinic in rural areas. The management of the medical and sanitary activities of the FAP is carried out by the health authorities. FAP conducts medical and preventive, sanitary and epidemiological work and sanitary and hygienic education of the population; has its own estimate, round seal and stamp indicating its name; draws up plans, a report with an explanatory note of the morbidity analysis; keeps accounting and reporting documentation. A feldsher (feldsher-midwife) with a completed secondary medical education is appointed to the position of the head of the feldsher-obstetric station. At the feldsher-obstetric center located in the village (where there is no pharmacy), a pharmacy (or kiosk) is organized to sell finished medicines and patient care items to the population.
Job responsibilities of the head of the FAP
Responsibilities of the head of the FAP (paramedic). The head of the FAP (paramedic) is in charge of organizing and planning medical and preventive care at the site; bears responsibility for the provision of timely medical (first-aid) care for various acute diseases and accidents.
The paramedic is obliged:
1) know the peculiarities of the organization of emergency care in case of mass accidents, poisoning with chemicals and drugs;
2) know the basics of pre-medical resuscitation; produce closed heart massage and artificial ventilation;
3) carry out outpatient reception and service of patients at home;
4) promptly send patients for consultation to the nearest medical and preventive institution (central district hospital);
5) if necessary, accompany the patient personally.
The paramedic organizes the reception of patients by district doctors and other specialists at the FAP according to the schedule approved by the chief physician. By the day of admission, the paramedic prepares the patients and the primary documentation. The doctor is receiving patients together with a paramedic. The personal participation of a paramedic in consulting patients contributes to the timely treatment of patients, their employment and advanced training of a paramedic.
The paramedic takes an active part in the prophylactic medical examination of the population of his area, draws up maps for patients subject to dispensary observation. A medical assistant under the direction of a doctor periodically organizes medical examinations of the population with unfavorable working conditions. Patients with tuberculosis, hypertension, ischemic heart disease, peptic ulcer of the stomach and duodenum, diabetes, glaucoma, thrombophlebitis, obliterating endarteritis, etc. are subject to dispensary observation. Chernobyl nuclear power plant. For the correct organization of the work of the FAP, a plan of treatment and preventive measures for the current year is drawn up. The plan specifies the planned activities, the deadline, the responsible executor. A pre-developed plan is approved by the chief physician. All planned activities are carried out on time.
The paramedic carries out medical control over the development and health of children in nurseries, kindergartens, orphanages, schools located in the territory of FAP and do not have the corresponding secondary medical workers in their states according to the approved plan, conducts sanitary-anti-epidemic and sanitary-educational work.
Organization of emergency care
To provide emergency care, first-aid resuscitation at the FAP, according to the approved report card, there must be a necessary set of instruments, dressings and medicines. In the emergency room there is a bed with a shield or a flat rigid couch, a stretcher, means of immobilization, a cabinet for storing medicines, a table, a sterilizer, syringes (2, 5, 10, 20 ml), rubber bands, a tonometer, a thermometer, probes of various sizes and funnel for gastric lavage, stethoscope, beakers, bucket, basin, set of rubber catheters, dressings, breathing and oxygen equipment, incubation set, oxygen cylinder.
Organization of medical care for the rural population
Obstetric and gynecological care for the rural population
The peculiarities of the living and working conditions of the rural population, expressed in the dispersion of settlements, the difference in the forms of organization of agricultural production, the variety of types of agricultural work (agriculture, animal husbandry, poultry farming, etc.), the large front of these works, their seasonality, determine the features of the organization of all medical care in rural area, including obstetric and gynecological.
Obstetric and gynecological care for the rural population is provided by a complex of medical and preventive institutions. Depending on the degree of approach to the rural population, on the specialization and qualifications of medical care, the level of material and technical equipment in the system of providing obstetric and gynecological care, it is customary to distinguish three stages.
Stages of providing obstetric and gynecological care
The first stage is the implementation of pre-medical and first medical aid. This stage is the rural medical area. It includes a rural district hospital with an outpatient clinic and a hospital, feldsher-obstetric points (FAP), and maternity hospitals. The location of the first stage is the periphery of the district.
The second stage is the implementation of qualified medical care. It includes district (numbered) and central district hospitals, which include obstetric and gynecological departments and women's clinics. The location of the second stage is the regional center.
The third stage is providing the rural population with highly qualified (specialized) obstetric and gynecological care. It includes a regional (regional, republican) hospital, which includes obstetric and gynecological departments and an antenatal clinic or an independent maternity hospital with an antenatal clinic. The location of the third stage is the regional (regional, republican) center.
Medical obstetric and gynecological care
Medical obstetric and gynecological care in a rural medical area is carried out by a general doctor - the chief doctor of a rural district hospital (if there are two doctors in a district hospital, one of them). Under his direct supervision, the midwife of the district hospital works, who helps the doctor both in the hospital (takes part in the management of childbirth) and in the outpatient clinic (takes part in monitoring pregnant women, postpartum women and treating gynecological patients). The number of maternity beds in a rural district hospital usually does not exceed 3–5. To bring qualified medical care closer to rural residents, the number of maternity beds in rural district hospitals is being gradually reduced and the number of beds in district and central district hospitals is expanding. However, in a number of districts, where, due to local conditions, it is not possible to provide the population with obstetric and gynecological care in district and central hospitals, rural district hospitals are being consolidated, and in accordance with this, the number of maternity beds is expanded to eight, and the post of an obstetrician-gynecologist is provided.
Pregnant women and women in labor with a pathological course of pregnancy and childbirth and a burdened obstetric history should not be hospitalized in a local hospital (in the absence of a specialist obstetrician-gynecologist on the staff).
Despite the presence on the periphery of the district of a medical hospital - a rural district hospital, the bulk of obstetric and gynecological care in a rural medical area refers to first aid, and it is carried out by midwives of the feldsher-obstetric station and the collective farm (inter-collective farm) maternity hospital. The work of these institutions is carried out under the direct supervision of the chief physician of the rural district hospital. If there is an obstetrician-gynecologist on the staff of the district hospital, the latter provides all medical and consultative assistance at the feldsher-obstetric station and in the collective farm maternity hospital.
FAP: structure of work
Feldsher-obstetric points (FAP) are provided by the nomenclature of medical institutions. FAP is organized in a village with a population of 300 to 800 residents in cases where there is no rural district hospital or outpatient clinic within a radius of 4–5 km.
All the work of the FAP is provided by a paramedic, a midwife, a nurse. The number of service personnel is determined by the capacity of the FAP and the size of the population served by it.
The FAP provides the following positions:
1) paramedic - 1 position with a population of 900 to 1300 people; 1 position with a population of 1300 to 1800 people; 1.5 positions with a population of 1800 to 2400 people and 2 positions with a population of 2400 to 3000 people;
2) nurse - 0.5 positions with a population of up to 900 people and 1 position with a population of over 900 people.
Depending on local conditions, the FAP may only conduct outpatient appointments or have maternity beds. In the latter case, along with outpatient care, the FAP is also inpatient.
Due to the fact that the FAP provides medical assistance to the entire rural population, and not only to women, the premises in which it is located should consist of two halves: paramedic and obstetric.
Obstetric unit of FAP
The obstetric part of the FAP should have the following set of premises: entrance hall, waiting room and midwife's office. FAPs with maternity beds, in addition to these premises, must have an examination room, delivery and postnatal wards. The FAP midwife carries out all the work on the organization and provision of obstetric and gynecological care to rural women within the radius of the service point.
Responsibilities of a FAP midwife
The responsibilities of a FAP midwife include:
1) identification of all pregnant women in the service area as early as possible, provision of dispensary observation of them, including the implementation of the necessary therapeutic and preventive measures, patronage of pregnant women, postpartum women and children under the age of 1 year;
2) carrying out sanitary and educational work among women;
3) providing medical care for normal childbirth;
4) identifying gynecological patients, referring them to a doctor and providing them with medical assistance as prescribed by a doctor.
Population bypasses
Significant assistance in the early detection of pregnant women is provided by household rounds of the population, carried out by a FAP midwife. In the observation of pregnant women, the midwife performs the entire bulk of the necessary research. So, at the first visit of a pregnant woman, the midwife collects a detailed anamnesis, general (heredity, past diseases, etc.) and special obstetric (menstrual, sexual, generative, lactation functions, gynecological diseases, etc.).
From the anamnesis, the midwife finds out the features of the course of previous pregnancies, the presence of extragenital diseases and other abnormalities in the woman's health that could affect the course of pregnancy and childbirth.
Examination of pregnant women
The midwife begins the examination of each pregnant woman with a study of internal organs: cardiac activity, blood pressure measurement (on both hands), pulse analysis, urine for protein (by boiling). The midwife is currently studying the state of health of pregnant women on the basis of measuring height, body weight (in dynamics), the presence of edema, pigmentation, the state of the mammary glands and nipples, and the state of the abdominal press.
Conducting a special obstetric examination, the midwife measures the external dimensions of the pelvis, by means of a vaginal examination, sets the gestational age and the internal dimensions of the pelvis. In the second half of pregnancy, it measures the height of the fundus of the uterus above the bosom, determines the position and presentation of the fetus, and listens to its heartbeat.
For a general blood test, group affiliation, determination of the Rh factor, antibody titer, Wasserman reaction, general urine analysis, the pregnant woman is sent to the nearest laboratory. Here, a bacteriological study of the vaginal flora is carried out for the degree of purity, the discharge of the urethra, cervix and vagina for gonococcus, the reaction of vaginal secretions. X-ray examinations in pregnant women (fluoroscopy of the chest, fetus, pelviography, etc.) are performed only if there are strict indications.
A thorough examination of pregnant women makes it possible to identify various pathological conditions, on the basis of which these pregnant women are allocated to high-risk groups and require the most close attention to them during pregnancy; in childbirth and the postpartum period, groups of increased risk are distinguished for cardiac pathology, bleeding in the postpartum and early successive periods, inflammatory-septic complications after childbirth, endocrinopathies: diabetes mellitus, obesity, adrenal insufficiency and other types of obstetric and somatic pathology.
All individual cards of pregnant women belonging to the risk group are usually marked with the appropriate color marking, indicating in a certain color the risk of a particular pathology (red - bleeding, blue - toxicosis, green - sepsis, etc.).
The volume of studies of gynecological patients
The scope of studies of gynecological patients also includes the collection of general and special gynecological anamnesis. The study of the state of health of women is currently carried out on the basis of a general clinical examination, similar to the examination of pregnant women. Special gynecological examination includes two-handed and instrumental (examination in mirrors) examination. A bacterioscopic examination of the discharge of the urethra, cervix and vagina for gonococcus is carried out using methods of provocation, according to indications - the Borde-Zhangu reaction; examination of a vaginal smear for cell atypia; research on tests of functional diagnostics.
If it is necessary for a woman to conduct a biochemical blood test for cholesterol, bilirubin, sugar, residual nitrogen and urine tests for acetone, urobilin, bile pigments, she is sent to the nearest multidisciplinary laboratory. Women and married couples who have a history of hereditary diseases or children with deformities of the central nervous system, Down's disease, cardiovascular defects are sent for examination, including for the determination of sex chromatin, to specialized medical genetic centers. While monitoring pregnant women, the FAP midwife is obliged to show each of them to the doctor. If a woman's pregnancy is proceeding normally, then her meeting with a doctor is carried out at her first scheduled visit to the FAP. All pregnant women who show the slightest deviation from the normal development of pregnancy should be immediately referred to a doctor.
At each subsequent visit to the FAP, the pregnant woman undergoes the necessary re-examinations. In the second half of pregnancy, it is especially necessary to carefully monitor the possible development of late toxicosis, for which it is necessary to pay attention to the presence of edema, the dynamics of blood pressure and the presence of protein in the urine. It is very important to monitor the dynamics of the weight of the pregnant woman.
Organization of patronage work
An obligatory section of the midwife's work in monitoring pregnant women should be conducting classes on their psycho-preventive preparation for childbirth.
In organizing monitoring of pregnant women in the countryside, as well as in the city, patronage work is very responsible. Patronage of pregnant women and gynecological patients is an element of the active dispensary method. The goals of patronage are very diverse, so each patronage visit to a woman sets a specific goal. First of all, this is an acquaintance with the living conditions of a woman. Knowing the peculiarities of the life of each family (housing conditions, family composition, level of material security, degree of culture, including health literacy, etc.), it is easier for a midwife to monitor the health of the population. The purpose of patronage is the need to find out the state of health of a pregnant woman who does not appear at the appointment at the appointed time. In this case, the midwife, in a conversation with the pregnant woman, finds out the general condition of the woman, makes a thorough examination, draws attention to the presence of edema, and measures blood pressure. With long periods of pregnancy, it measures the circumference of the abdomen and the height of the uterine fundus, determines the position of the fetus. After making sure that there are no deviations from the normal development of pregnancy, the midwife appoints the woman a deadline for the next examination. In the presence of the slightest signs of complications of pregnancy, the midwife invites the pregnant woman to an appointment with the doctor or informs the doctor about it, who decides on the possibility of treating the pregnant woman at home or the need for her hospitalization. In the latter case, the midwife monitors the timeliness of the woman's admission to the hospital and continues active monitoring after her discharge home. The reason for the patronage may be the desire to make sure that the woman fulfills the doctor's prescriptions correctly, the need to conduct additional research (laboratory tests, measure blood pressure, etc.).
The FAP midwife is obliged to provide patronage of children, especially the first 3 years of life. At the same time, it is necessary to observe the frequency of observations of children of the 1st year of life by the midwife (paramedic) of the FAP: 1st month of life - observation only at home - 5 times; 2nd month of life - observation at home - 3 times; 3-5 months of life - supervision at home - 2 times a month; 6-12 months of life - observation at home - once a month. In addition, a child under 1 year old should be examined by a pediatrician at the FAP at least 1 time per month.
Thus, the midwife sees the child during the first year of life 12 times during preventive examinations by a doctor and 20 times during home patronage.
The midwife's patronage work is strictly planned. The plan provides for the days of visiting villages and villages. In a special notebook, a record of patronage work is kept, all visits by women and children are recorded. The midwife enters all the advice and recommendations into the home visiting nurse's notebook of work at home (patronage sheet) for subsequent verification of their implementation.
Mobile teams from the Central District Hospital
The bulk of women from rural areas give birth in medical obstetric departments of the Central District Hospital. If necessary, inpatient qualified medical care is provided to rural women in large republican, regional, regional maternity hospitals.
To bring ambulatory and polyclinic medical care closer to rural residents, mobile teams from the Central Regional Hospital are being created, which come to the feldsher-obstetric stations according to the approved schedule.
The mobile team includes an obstetrician-gynecologist, pediatrician, therapist, dentist, laboratory assistant, midwife, children's nurse. The composition of the mobile team of doctors and paramedical workers is brought to the attention of the heads of the feldsher-obstetric centers.
Conducting preventive periodic examinations
The paramedic and midwife are required to have a list of women in their area who are subject to preventive and periodic examinations.
Practically healthy women with a successful obstetric history, a normal course of pregnancy in the period between team visits are observed by a FAP midwife or a local hospital, and are sent for childbirth to the nearest local or district hospital.
With a group of women who are contraindicated in carrying a pregnancy, an obstetrician-gynecologist and a midwife conduct conversations about the harm to their health of pregnancy, possible complications of pregnancy and childbirth, teach them to use contraceptives, and recommend intrauterine contraceptives. The obstetrician-gynecologist of the mobile team checks the obstetrician-gynecologist's fulfillment of appointments and recommendations during the second visit. Household visits conducted by a midwife provide significant assistance in the early detection of pregnant women. All identified pregnant women, starting from the earliest stages of pregnancy (up to 12 weeks), and postpartum women are subject to medical examination.
In the normal course of pregnancy, a healthy woman is recommended to visit a consultation with all the analyzes and conclusions of doctors 7-10 days after the first visit, and then visit a doctor in the first half of pregnancy once a month, after 20 weeks of pregnancy - 2 times a month, after 32 weeks - 3-4 times a month. During pregnancy, a woman should visit the consultation about 14-15 times. In case of a woman's illness or a pathological course of pregnancy that does not require hospitalization, the frequency of examinations is determined by the doctor on an individual basis. It is important that pregnant women attend the consultation carefully during antenatal leave.
Hospitalization of pregnant women in medical hospitals
Timely hospitalization of pregnant women in medical hospitals when initial signs of deviation from the normal course of pregnancy appear, as well as women with a burdened obstetric history, is very important in the work of a FAP midwife. Pregnant women with a narrow pelvis (with external conjugate less than 19 cm), abnormal position of the fetus and breech presentation, immunological incompatibility of the blood of the mother and the fetus (including history), extragenital diseases, with the appearance of bloody discharge from the genital tract are subject to prenatal hospitalization in medical hospitals , edema, the presence of protein in the urine, increased blood pressure, excessive weight gain, in the establishment of multiple pregnancies, as well as in other diseases and complications that threaten the health of a woman or child.
When sending a pregnant woman to an obstetric hospital, it is very important to choose the right way of transporting her (ambulance, air ambulance, passing transport), as well as to correctly resolve the issue of the institution in which this pregnant woman should be hospitalized. A correct assessment of the state of health of a pregnant woman will allow avoiding multi-stage hospitalization, and will immediately identify the patient to that obstetric hospital where there are all conditions for providing her with full medical care.
Delivery at FAPAt the feldsher-obstetric station, only normal (uncomplicated) childbirth is provided. In cases where a complication occurs during childbirth (which cannot always be foreseen), the FAP midwife should immediately call a doctor or (if possible) take the woman in labor to a hospital. In this case, it is very important to resolve the issue of means of transportation. It must be remembered that women with an unseparated afterbirth, preeclampsia and eclampsia, as well as with a threatening uterine rupture, cannot be transported. If a woman with an unseparated placenta needs transportation due to certain complications of pregnancy, the FAP midwife must first of all perform manual separation of the placenta and transport the woman with a contracted uterus. If it is impossible to provide a woman with the necessary assistance to such an extent that she is in a state of transportability, you should call a doctor to her and outline a plan for further action with him. Providing emergency first aid to a pregnant and giving birth woman, the FAP midwife has the right to perform the following obstetric operations and benefits: turning the fetus on the leg with full opening of the uterine pharynx and whole or just departed waters, removing the fetus by the pelvic end, manual separation of the placenta, manual examination of the uterine cavity , restoration of the integrity of the perineum (after rupture of the perineum or perineotomy). With bleeding in the early postpartum period, the midwife must exclude rupture of the tissues of the birth canal. Complications arising during childbirth require from the midwife, in addition to urgently calling a doctor, clear organizational actions, on which the outcome of childbirth largely depends. The midwife should be fully proficient in the primary methods of resuscitation of newborns born with asphyxiation.
FAP documentation
It is very important in the work of a FAP midwife to maintain thorough documentation. For each pregnant woman applying to the FAP, an “Individual card of a pregnant woman” is filled out. When obstetric complications or extragenital diseases are detected, a duplicate of this card is filled in, which is transferred to the district obstetrician-gynecologist.
There are many options for storing individual cards. One of the most convenient options for work, which can be recommended, is as follows: the box for storing individual cards (the width and height of the box must match the size of the card) is divided by transverse partitions into 33 cells. Each partition is marked with a figure from 1 to 31. These figures correspond to the dates of the month. When appointing the next visit to the pregnant woman, the midwife places her card in the box with the corresponding date of the month, that is, the day when she needs to appear for the appointment. Before starting work, the midwife takes out all the individual cards from the cell corresponding to the day of reception and prepares them for admission: they will check the correctness of the entries, the availability of the latest tests, etc. corresponding to the day of the month for which she is scheduled to attend. At the end of the appointment, by the number of cards remaining, it is easy to judge about pregnant women who did not show up for an appointment on the day assigned to them. The midwife places these cards in the 32nd cell of the box marked "Patronage". The midwife then visits (patronizes) all women who do not attend. All cards of those who have given birth and are subject to dispensary observation until the end of the postnatal period are placed in the 33rd cell with the mark "Postpartum women".
In addition to these documents, the FAP maintains a diary-notebook of entries for pregnant women (f-075 / y) and a diary (f-039-1 / y). When a pregnant woman (after 28 weeks of pregnancy) or a postpartum woman is sent to a medical obstetric hospital, an "Exchange card" is issued to her. If a pregnant woman is hospitalized before 28 weeks, an extract from the medical history is issued to her. When she is discharged from the hospital, she receives an extract from the medical history in the same form, which is given to her by the FAP midwife.
Organization and implementation of preventive examinations of rural women
An important section in the work of a midwife of a feldsher-obstetric station is the organization and conduct of preventive examinations of women. It is advisable to carry out preventive examinations of rural women in the autumn-winter period in order to complete the rehabilitation of the identified patients before the spring field work.
All work on the organization of preventive examinations is supervised by the district obstetrician-gynecologist and the chief midwife of the district. A preliminary plan for conducting inspections is drawn up, which indicates the place where the inspection will be carried out, the calendar dates of inspections for each locality. Preventive examinations are carried out by FAP midwives who have undergone special training and instruction. For a successful preventive examination, the midwife must first make a home visit, the tasks of which are to explain to women the purpose of the examination, the method of its conduct, the place of examination, etc.
The purpose of preventive examinations is the early detection of precancerous, neoplastic, inflammatory and so-called functional diseases of the genital organs in women and the appointment, if necessary, of appropriate treatment. Preventive examinations also make it possible to identify occupational hazards among the organized part of the female population that affect the organs of the genital area, and to develop measures to eliminate them.
Direct examination of women consists of two sequential procedures:
1) examination of the external genital organs, the vagina and the vaginal part of the cervix (using mirrors);
2) two-handed research in order to clarify the state of the internal genital organs.
During preventive examinations, objective diagnostic methods are used: cytological examination of the vaginal discharge, "prints" from the cervix, colposcopic examination.
To carry out laboratory research, material is taken from various departments of the woman's urogenital apparatus:
1) smears from the urethra and cervical canal for bacteriological examination for Neisser's gonococci and flora. The material obtained from the urethra is applied to the glass slide in the form of a circle, and from the cervical canal - in the form of a stroke in the longitudinal direction;
2) a smear from the posterior fornix of the vagina to determine the degree of purity of the vaginal contents is taken after the introduction of the mirrors;
3) a smear from the lateral wall of the vagina for hormonal cytodiagnostics is also taken after the introduction of the speculum.
At the slightest suspicion of a disease that has arisen in a midwife performing a routine examination, a woman should be immediately referred to a doctor.
In conducting preventive examinations, careful registration and registration of all examined women is very important, for which a list of persons subject to targeted medical examination for identification is drawn up. For registration and accounting of women subject to active dispensary observation, dispensary observation control cards are entered on them.
Another institution that provides pre-medical obstetric and gynecological care in rural areas is the collective farm maternity hospital. In a collective farm maternity hospital, the following premises must be provided: vestibule, reception room, delivery room (10–12 m2), postnatal ward (6 m2 for 1 maternal and child bed), kitchen, toilet. Each collective farm maternity hospital has 2 to 5 beds (at the rate of 1 bed per 1000 population).
A collective farm maternity hospital is located at a distance of 6-8 km from the rural medical area to which it is attached. With good transport conditions, this distance can be increased to 10-15 km. Collective farm maternity hospitals are served by a midwife, whose duties are similar to those of a FAP midwife. If in one village near the FAP there is a collective farm maternity hospital and there is no need for an independent staff in terms of the volume of its work, the service of the latter is assigned to the FAP midwife.
Occupational safety issues in the work of the obstetric and gynecological serviceIn the work of the obstetric and gynecological service in the countryside, at all its stages, a lot of space is occupied by issues of labor protection of female workers in agricultural production. Agricultural work has its own characteristics, the main of which are seasonality, the performance of various production operations in a short time in any weather conditions, etc. This requires considerable effort and stress from a person, which inevitably leads to violations of the regime of work and rest. Agricultural workers experience additional adverse effects of such production factors as noise, vibration, dust, contact with pesticides (pesticides) and mineral fertilizers. The main work on the implementation of measures aimed at labor protection of rural residents is carried out by hygienists. But the obstetric and gynecological service should also take part in this work, since unfavorable production factors also have a negative effect on the specific functions of the female body.
From the book The Complete Medical Reference of a Paramedic author Vyatkina P.Chapter 1 Independent work of a paramedic in an ambulance and as part of a paramedic-medical brigade Organization of work of an ambulance The ambulance service is one of the most important links in the health care system in our country. Volume
From the book Own Counterintelligence [Practical Guide] author Zemlyanov Valery MikhailovichPart II Basic principles of the work of a paramedic in a paramedic and obstetric
From the book Woman. Guide for men author Novoselov Oleg OlegovichPart III Basic principles of operation
From the book Fundamentals of Competitiveness Management author Mazilkina Elena Ivanovna From the book Woman. A textbook for men. author Novoselov Oleg Olegovich From the book A Million Dollar Story author McKee RobertChapter 2. hierarchical structure
From the author's book1.5 Primitive tribe. Functional structure. Hierarchy structure. The structure of intersexual relations Even the most primitive peoples live in a culture different from the primary one, temporarily as old as ours, and also corresponding to a later one,
From the author's bookCHAPTER 3. STRUCTURE AND SETTING THE WAR WITH STAMPS Perhaps, for the entire period of human existence, today it is the most difficult for a writer to work. Compare today's story-fed audiences with those of the past. How many times a year educated people
From the author's book